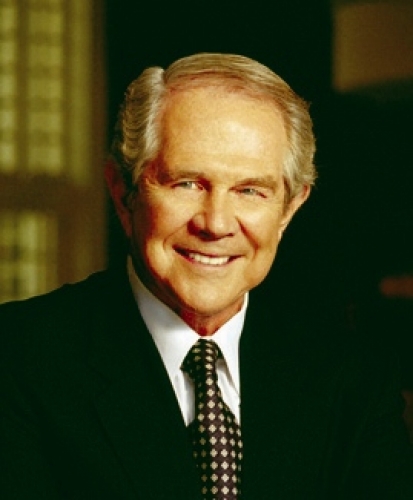
Pat Robertson is used to receiving messages from above. But never had such guidance come from a surgical-equipment salesman flying at 30,000 feet. Nor had it ever been advice to fix the preacher’s ailing heart.
Robertson, founder of the Christian Broadcasting Network, was diagnosed with atrial fibrillation in 2004. “It’s a terrible thing, when it comes upon you,” he says. “You’re very short of breath, and it just saps the life out of you.”
Atrial fibrillation, also known as A-fib, is the most common form of irregular heartbeat; it occurs when errant electrical signals disrupt the normal signals that regulate the heart. The result is diminished blood flow, which causes symptoms like those Robertson suffered, as well as increased risk of stroke.
“I remember once I had to do a telethon, which is long, hard work,” Robertson says. “I was so exhausted that I could hardly hold onto the platform in front of me. Unless somebody’s had it, they don’t understand how debilitating A-fib can be.”
He tried several medications over the years, but they all eventually failed him. His doctor suggested a cardiac ablation—inserting a catheter with an electrical probe through an artery and into the heart to deaden misfiring cells. At first, it worked. But months later Robertson was back in A-fib. Doctors tried an ablation again, and again it failed.
Robertson implored his doctors to try something else. The only real option, they said, was to shock his heart back into the proper rhythm.
“They put you under anesthesia, and then they shock you,” Robertson says. Once again, the problem was only solved temporarily. “I wound up having this procedure seven or eight times—about every four or five months,” he says. “I was there so often that the folks in the hospital began calling the machine the Pat-Zapper.”
That’s when he received the life-changing message from above.
“A friend of mine happened to sit next to a surgical-equipment salesman on an airplane,” Robertson says. “He told my friend about this surgeon in North Carolina who invented a procedure to correct A-fib. My friend urged me to call the surgeon, and that’s how I met Andy Kiser.”
New route to the heart
For years, the last-ditch treatment for A-fib has been the “cut and sew” maze procedure—surgeons cut open the chest to create scar tissue on the heart muscle, which disrupts the abnormal electrical impulses. Lengthy and complicated, the maze procedure is used rarely because it’s also invasive and risky.
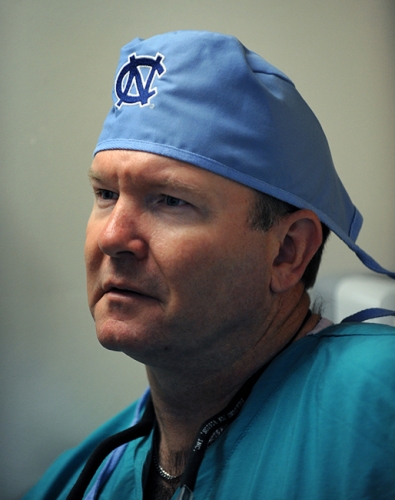
Kiser, a cardiothoracic surgeon at UNC, developed a different approach using a new, more effective ablation device to deaden misfiring cells. The results were amazing, he says, but the procedure still required open-heart surgery, which always poses a risk of complications.
“I wanted to treat atrial fibrillation without opening the chest,” Kiser says. “One day, I was repairing a para-esophageal hernia, and I had to cut through the diaphragm in order to access the hernia. I realized that I could see the back exterior of the heart from that angle. I thought, ‘Man, that’s the way to do it!’”
Kiser came up with a new device that could be inserted through a small incision above the liver and, from there, through the diaphragm. “With this,” he says, “I could see the exterior of the heart and create scars on its surface without opening up the entire chest.”
But Kiser knew that the procedure, as he conceived it, could only target the outside surface of the heart. He needed someone trained to treat the inside of the heart. Kiser enlisted his colleague, cardiologist Mark Landers, to perform an ablation on the interior of the heart via a catheter at the same time Kiser would treat the surface of the heart. This convergent approach, Kiser thought, would ensure better ablation coverage, which he hoped would significantly improve or even cure A-fib.
The results have been impressive; Kiser and his team are achieving a 70 to 80-percent success rate. The convergent technique is now being used to treat A-fib patients around the world who have run out of other treatment options. Pat Robertson was one of the successes; after a nine-year battle and Kiser’s procedure, Robertson is able to control his A-fib with minimal medication.
Convergent colleagues
To Kiser, collaboration is key to the procedure’s success.
“Until we started doing this kind of collaboration,” Kiser says, “cardiothoracic surgeons and cardiologists really didn’t work together. We sort of did our own things. Putting them in the operating room at the same time and expecting them to work together to solve a problem? That just did not happen.
“But today, we’re collaborating to do certain kinds of valve replacements, pacemaker removals, and ablations to correct ventricular tachycardia.”
The success of this new, minimally invasive team approach has had a ripple effect. “We’re being approached by industry people with new products and devices that they want us to test. They want us to help them develop device-training programs,” Kiser says.
One of those new devices is a tiny pump that helps failing hearts move blood. The CircuLite Synergy, as it’s called, assists patients who don’t yet qualify for a heart transplant but are no longer responding to medical therapies. Because it’s small—no larger than a double A battery—the device can be implanted easily.
“Twenty or thirty years ago, there was no ‘less invasive’ surgery of any kind,” says Filip Rega, a cardiothoracic surgeon in Belgium who has studied the effectiveness of CircuLite’s pump overseas. “That remained true for cardiac surgery until very recently. There was no less-invasive way to enter the heart and achieve the same effects as in open-chest surgery. But all that’s changing now.”
Rega visited North Carolina in 2012 to tour the cardiac surgery training program Kiser set up at UNC and to solicit Kiser’s help teaching cardiothoracic surgeons how to implant the CircuLite pump.
“The size of CircuLite’s pump means that it needs to be placed differently than other heart-assist devices,” explained Rega. “Cardiac surgeons have to learn to think differently about using it—such as identifying the ideal recipients, knowing how to place the pump, and understanding what complications might arise due to patient variability.”
The CircuLite Synergy was approved for use in Europe in September 2012 after five years of testing. The company is now seeking FDA approval for a clinical trial in the United States. Kiser is instrumental in this; he’s setting up a training program for American cardiothoracic surgeons who will want to use the new technology.
Moreover, in 2011 Kiser established a five-year partnership with the company KARL STORZ Endoscopy that will enable UNC’s School of Medicine to use STORZ’s technology for training and development.
The company believes that minimally invasive surgery is the optimal approach whenever possible. But many experienced surgeons and medical students aren’t taught newer, less invasive techniques. Yet, such techniques tend to produce more successful health outcomes, fewer complications, and shorter hospital stays.
Kiser sees the KARL STORZ Center of Excellence as a model of collaboration between industry and the medical community.
“Surgeons have to learn new skills all the time, especially as medical technology advances,” he says. “Companies developing new devices want to make sure that their technologies are used correctly and that patients have good outcomes. A great way to do that is to educate surgeons in a simulation environment like our center and show them how to do it correctly.”
Something Bigger
“This program isn’t about going to the operating room, doing cases, and making a lot of money that goes into our pockets,” Kiser says. It’s about something bigger than that. “We have to fund medical education, and we cannot do that alone. We have to use our current resources to generate funds that can then be reinvested into education and training.”
In addition to the fees from his training endeavors, Kiser has generated support by contracting with the media, which can use his large library of procedure videos for television and online clips. He has also created a business-card-sized cardiac emergency kit—the A.C.E. for Hearts—that people can carry in their wallets and use if they think they may be having a heart attack and need immediate help.
So far, Kiser has raised nearly $100,000.
“We have to get outside of our normal practice and do something uncommon,” Kiser says.
It’s the team approach to research and clinical practice, he says, that has encouraged private companies to invest in training doctors.
“At the same time, we’re able to help them by training people to do new procedures and use their new medical devices,” Kiser says.
At the heart of it all, though, are the patients; they benefit the most.
“These collaborations,” Kiser says, “present a world of opportunity for doing good.”
Andy Kiser is a professor of surgery and chief of the Division of Cardiothoracic Surgery in the School of Medicine. He was chief of cardiovascular and thoracic surgery at First Health-Moore Regional Hospital in Pinehurst, North Carolina, when he developed the convergent procedure with electrophysiologist Mark Landers.
Brenda Denzler is a communications specialist for the Medical Foundation of North Carolina, Inc.