It happens more than you’d think. A person eats a bit too fast and gets a hotdog stuck in his throat. He chugs water, swallows hard, but can’t get that darned dog down. He isn’t choking, but he feels like he is: the lodged food in the esophagus, which is next to the windpipe, causes a sensation of troubled breathing. He goes to the emergency room, where doctors stick an endoscope down his throat to clear the esophagus. Problem solved? Maybe not.
“About 50 percent of people in that situation have eosinophilic esophagitis,” says Evan Dellon, a gastroenterologist at UNC.
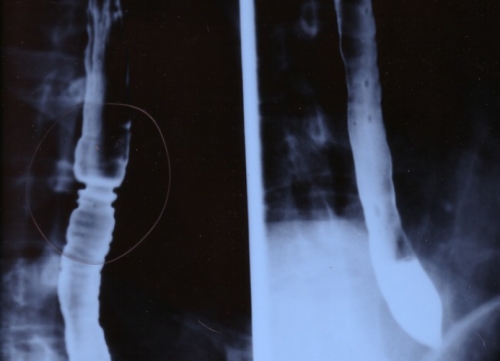
Wikimedia Commons
At left, an x-ray of an esophagus stricken with Eosinophilic Esophagitus, also known as EoE, a new disease usually coased by food allergies. The main symptom: difficulty swallowing.
Click to read photo caption. Wikimedia Commons
Eo-what? Let’s call it EoE, as researchers do. It’s caused by allergic reactions, mostly to food. The reactions cause inflammation, which over time causes scar tissue, which narrows the esophagus, which makes swallowing difficult.
Most people with EoE go years without knowing they have it. Dellon says they often compensate by chewing food very slowly until it turns to mush, making it easier to swallow. That strategy can work for a while, Dellon says, but eventually careful eating won’t suffice. The esophagus will become so narrow that one day the proverbial hotdog will get stuck. And then it’s off to the emergency room.
Dellon is UNC’s EoE expert. He’s been studying the disease since the day he first heard about it, which wasn’t that long ago: EoE is the newest esophageal disease on the scene. And though it’s not nearly as serious as cancer or as common as acid reflux, EoE is on the rise and could be life-threatening.
EoE didn’t exist when Dellon was in medical school in the 1990s. Doctors documented a few strange cases of esophageal problems, but the condition was not well-defined. Even when Dellon entered residency in 1999, EoE still wasn’t well-documented.
He first read about it in 2004, when he was a GI fellow at Carolina. Part of his training required him to be on call for emergencies. “I kept seeing these patients who had food stuck in their throats,” he says. “They swallowed and swallowed, but the food wouldn’t go down.”
Dellon knew that the more a person in this situation tries to swallow—the more the esophagus squeezes and contracts—the more likely that the esophagus will rupture. And that can leach all sorts of nasty stuff, including bacteria, into the chest cavity, risking infections of vital organs. “That’s life-threatening,” Dellon says.
The emergency solution to lodged food is an endoscopy—inserting into the throat a long tube with a lens at the end. Once the food is pushed down, people feel better and assume they should just be more careful. But as Dellon consulted with patients, he realized that most of them had been having trouble swallowing for years.
“I began to look into this a bit,” he says. In the medical literature he found research describing a new disease characterized by esophageal scar tissue, difficulty swallowing, and the presence of white blood cells called eosinophils, which are part of the immune system and are found throughout the GI tract but aren’t supposed to be in the esophagus.
“It seemed to me that this condition, EoE, was the most likely reason why people, mostly younger people, were getting food stuck,” Dellon says. But the literature still didn’t provide a clear path toward diagnosis.
Imagine if one doctor said a systolic blood pressure of 40 was too high but another said a pressure of 400 was too high. Diagnosing EoE is like that, except what varies is the number of eosinophils in the esophagus.
Dellon first documented this poor diagnostic roadmap for EoE patients in a 2007 paper, and he began working on ways to distinguish the disease from other upper GI conditions such as Gastroesophageal Reflux Disease—also known as GERD or acid reflux—which is much more common than EoE and also can cause difficulty swallowing.

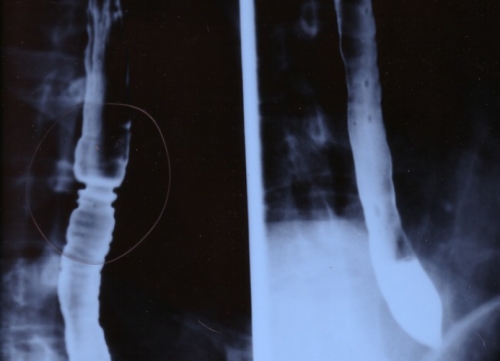
Wikimedia Commons
An endoscopic image of the rings inside an esophagus stricken with Eosinophilic Esophagitus, also known as EoE.

Click to read photo caption. Wikimedia Commons
Dellon found that, unlike GERD patients, EoE patients have white plaques in their esophagi. They’re typically much younger than GERD patients and include infants, they lack the GERD hiatal hernia where the esophagus and stomach meet, and their esophagi are ringed (see image), which means severe scar tissue has formed around esophageal muscles.
Most telling is that EoE patients in Dellon’s study typically had a much higher number of eosinophils—found in the airways of people with asthma and the skin of people who have eczema—and many EoE patients in Dellon’s study suffered from some kind of food allergy. That’s the key to this disease. Essentially, it’s an allergic reaction.
Dellon’s addition to the medical literature has helped doctors recognize EoE in patients who’ve been suffering for years. And as part of his duties at UNC, Dellon travels around North Carolina to spread the word about how to diagnose and treat EoE.
“For adults who want to treat the condition through diet, we recommend the six-food elimination diet,” he says. “Patients stop eating wheat, milk, nuts, seafood, eggs, and soy.” Then they slowly reintroduce the foods one at a time to pinpoint the allergen.
“About 50 or 60 percent of EoE patients are allergic to wheat or milk,” Dellon says.
If the allergen is found and the patient can avoid it, the esophagus will heal in a matter of weeks or months. If not—or if patients prefer taking medicine to altering their diet—then doctors prescribe topical steroids (an adapted use of asthma medication). EoE patients spray the steroids into their mouths and swallow so the medication coats the esophagus. “This works really well,” Dellon says. “There are nine randomized placebo studies documenting this approach in kids and adults.”
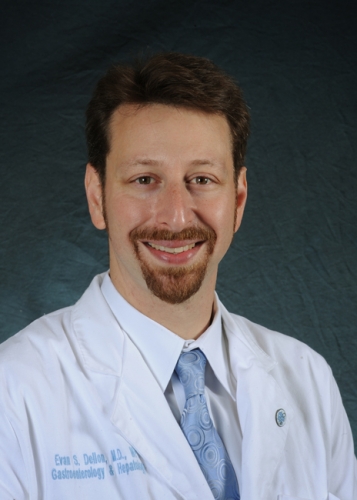
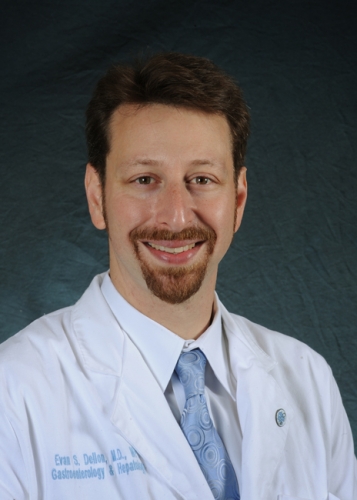
Photo credit: Dan Sears
Evan Dellon, one of four junior faculty awarded the Phillip and Ruth Hettleman Prizes for Artistic and Scholarly Achievement by Young Faculty.

Click to read photo caption. Photo credit: Dan Sears
One problem, though, is that asthma medication for EoE is an off-label use, which means insurance companies often won’t cover it.
“There’s a real need for other treatments,” Dellon says. “You can’t just rub a steroid cream on the esophagus like you can for skin eczema. So people are working on syrups and gel pills.”
So far, EoE is classified as a rare disease. The FDA estimates that fewer than 200,000 people have EoE in the United States. That’s a drop in the bucket compared to 80 million GERD sufferers. But EoE is clearly on the rise, Dellon says.
The good news is that unlike many other inflammatory diseases, such as GERD or Barrett’s Esophagus, EoE doesn’t seem to be a risk factor for esophageal cancer, one of the more deadly forms of cancer.
The bad news is that diagnosing EoE is still difficult. GERD and EoE aren’t the only diseases that cause problems with swallowing—so can infections, esophageal spasms, esophageal dysfunction, cancer, benign growths, and anatomical anomalies. Because EoE is such a new disease, doctors often rule out other possibilities before they consider EoE. Some doctors may not have even heard of it. In some patients it can take ten or more years before EoE is correctly diagnosed, Dellon says.
Only when doctors employ an endoscopy and take biopsies or tissue samples, which are costly procedures not without risk, can they confirm the diagnosis of EoE.
Dellon is trying to get around that by creating a blood test. “If we can measure specific factors found in EoE biopsies and compare them with factors found in the blood of patients,” he says, “then we could make a diagnosis without an endoscopy.
“This work is still in the early stages, but it’s promising, for sure.”