Pharmaceutical companies are coming up with more drugs to treat erectile dysfunction than to treat drug-resistant bacterial infections. “You can tell where the money is,” Scott Singleton says. The companies don’t think that antibiotics are a good investment, he says, because by the time they get a new antibiotic to the market and start paying off the high costs of research and development, bacteria might once again be a step ahead of the drugs.
Singleton and his lab are doing basic research on bacterial drug resistance and antibiotics, and their work could lead to a new drug that doesn’t need to pay off its costs. “We’re lucky,” Singleton says. “Our technology is being developed on NIH-funded grants.”
The real crux of the antibiotic-resistance problem is that we don’t know how bacteria become resistant. Scientists have worked out what bacteria do to beat drugs, but how they evolved to do those things in the first place and what drives that evolution is still a bit of a mystery. “Those mechanisms didn’t just arrive from aliens — they came from somewhere,” Singleton says. “So it occurred to us that if you could control those mechanisms you could slow down the rate at which bacteria evolve resistance.”
He and his lab work on an enzyme called RecA that’s in nearly all bacteria. RecA maintains and repairs a bacterium’s DNA. The closer Singleton looked into RecA, the more roles he saw it playing. It’s like an airline employee who does every job in the airport, he says. “You go there and a person takes your ticket. Then you see the same person take your luggage out to the plane, and pretty soon he’s flying the plane. RecA is like that,” Singleton says.
In most bacteria, RecA monitors single-stranded DNA, which usually exists only for brief moments, such as when the DNA is replicating, before it goes back to its double-helix structure. But if a bacterial cell encounters harsh drugs or UV radiation, for example, its DNA can be damaged and break apart. RecA assesses the damage and patches the broken DNA by recombining other pieces of DNA to fill in gaps. If too much damage has occurred, RecA triggers an emergency system that generates new DNA to fill large gaps with speed, but not accuracy.
This sloppy DNA repair and recombining of fragments could allow bacteria to develop resistance to antibiotics. “We know that if we genetically engineer the bacteria to be without RecA, they’re much more sensitive to antibiotics,” Singleton says.
On top of that, scientists have also found that antibiotics cause DNA damage. Even though an antibiotic may do its work outside the bacterial cell, the drug causes changes inside the bacteria that lead to bacterial DNA damage. “That’s why RecA helps them survive,” Singleton says. When antibiotics attack, RecA is turned on, and it increases the mutation rate. More mutations might mean more resistance.
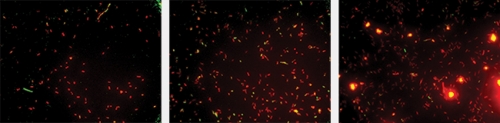
So Singleton did what a lot of drug companies would have done: he set up a screen for small molecules that could inhibit RecA. “I think we’ve screened about sixty-five thousand molecules,” Singleton says. The lab identified hundreds of RecA inhibitors.
“Finding the inhibitor is just the first step. Then you have to figure out how it works,” Singleton says. Some of the inhibitors may completely shut down RecA, while others only affect one of RecA’s jobs. And inhibiting each of RecA’s jobs will give Singleton clues about what RecA is doing and which jobs are most important. “Is it okay if nobody takes your ticket at the airport?” he asks.
To answer those questions, Singleton and his lab are doing biological and genetic experiments. “For us that was the challenge, because we’re chemists,” he laughs. In the meantime, he’s working closely with UNC’s Office of Technology Development to design a licensing agreement to develop the findings into a new drug.
The plan is to continue generating data on these small inhibitors, and maybe in the next twelve to eighteen months the project will have a confident investor. There is a catch, though — a part of the licensing Singleton is adamant about. “We carved out a piece of the licensing that will cover developing countries,” he explains. “The idea is simple — no pharmaceutical product manufactured in the United States will be sold for a profit in those places. Of all the things we sort of wrangled over, that was not one.
“The evolution of antibiotic resistance is making antibiotics useless and the places where that’s felt the hardest are developing countries,” Singleton says. In the United States it’s relatively rare to come across an infection that’s resistant to all the drugs in our arsenal, but in developing countries that’s not the case. “In a developing country you might only have access to a very limited number of drugs,” he says.
This is the kind of work that Singleton hoped he’d end up doing: helping people. “I always thought I’d be a doctor. My dad’s a doctor,” he says. “I sort of jumped all the way to pure, basic chemical research and I’ve been slowly moving back. I think a lot of my friends are still shocked that I’m interested in anything practical.”
Singleton says that his lab does research that won’t get done in the private sector. “It’s not the kind of thing a pharmaceutical company would focus on if it had to make a hundred million dollars next year selling something,” he says. “So, I think it’s exactly the kind of thing we should be focused on.”
Beth Mole was formerly a postdoctoral fellow in the medicinal chemistry and natural products division of the Eshelman School of Pharmacy.
Scott Singleton is an associate professor of medicinal chemistry and natural products in the Eshelman School of Pharmacy. Funding for his work came from the National Institutes of Health.The Office of Technology Development (OTD) is the only UNC office authorized to execute license agreements with companies. For information on reporting inventions, contact OTD at 919-966-3929.