If you eat yogurt, you eat bacteria. Billions of microbes per serving—Lactobacillus acidophilus, Streptococcus thermophilus, Bifidobacterium. They’re called probiotics and are supposed to help the naturally occurring “good” bacteria in our digestive tracts keep the “bad” bacteria in check. But do they do that for all of us? And how bad can those “bad” bacteria really get?
UNC scientists are starting to find out, and some of the news is a bit troubling.
Our bellies are rife with bacteria, even certain strains of Escherichia coli. But these E. coli are what scientists call commensal bacteria—we don’t bother them and they don’t normally bother us, because our digestive tracts are protected by our immune system and lined with a layer of mucus. But what if that layer is compromised?
That’s what happens to patients with inflammatory bowel disease (IBD). They suffer through chronic inflammation, which can lead to DNA damage, mutated colon cells, and cancer. IBD patients are seven times more likely to develop colon cancer than are people without IBD. Carolina researchers have already found that bacteria can trigger inflammation. But can bacteria trigger cancer? UNC microbiologists Christian Jobin and Janelle Arthur wanted to find out.
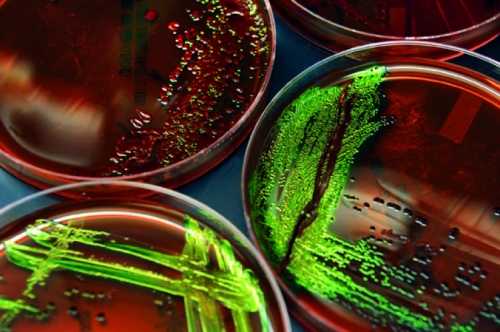
In their first experiment, they used two groups of mice that were genetically susceptible to developing IBD when put in contact with specific bacteria. Arthur exposed one set of these mice to a strain of commensal E. coli and another set of mice to commensal Enterococcus. Both groups of mice developed inflammation, but Jobin and Arthur found that only the E. coli mice developed cancer. “We thought, my God, there must be some specific part of the bacteria that fosters the disease,” Jobin says.
Ernesto Pérez-Chanona, a grad student in Jobin’s lab, searched the scientific literature and found that only a few bacterial genes in E. coli have been shown to damage human DNA. When Jobin’s team analyzed the genes of this specific E. coli species, they found only one known DNA damager—a string of genes encoded on what’s called a polyketide synthase island or PKS.
Jobin says that PKS is like a factory. It’s composed of 22 genes and produces colibactin, which is toxic to human cells.
With that bit of knowledge, Jobin and Arthur collaborated with UNC colleague Jonathan Hansen, who deleted the PKS gene factory in E. coli so the bacteria couldn’t produce colibactin. Then the researchers added the strain of E. coli to mice. When Arthur studied the mice, she found some precancerous cells in their colons—“some very early signs of something that looked off,” she says. “But we didn’t see huge tumors like we saw in the PKS mice.”
The odd thing is that all the mice—with or without PKS—had the same amount of inflammation, but the mice with PKS had more DNA damage, further evidence that the bacteria—not inflammation—were driving the cancer.
“We have a proof of principle that inflammation may not be sufficient to promote colon cancer,” says Jobin, whose team published its findings in the journal Science. Gut microbes have the ability to damage DNA and promote cancer.
Yet, genetically altered mice are far from being human.
“In animal models we control for everything,” Jobin says. “In humans, there are other factors. But if a person has continuous episodes of stress, poor diet, or inflammation—if microbes gain access to the gut lining because the mucosal layer is changed, and you have too many of these E. coli, then the E. coli could be another contributing factor for colon cancer.”
In fact, Jobin’s team found that patients with colon cancer have a higher prevalence of E. coli that contain the PKS gene factory than do people without colon cancer.
If these bad bugs could trigger cancer, then Jobin and Arthur wondered whether good bugs could prevent it.
The probiotics in yogurt and pills don’t naturally occur in your gut in high density. They don’t colonize, which is why some people take probiotics daily. Some studies have shown that probiotics can help alleviate gastrointestinal problems in people. And prebiotics—fibrous foods such as onions, garlic, and leeks—can promote beneficial bacteria that naturally occur in our digestive tracts. Several animal studies have shown that probiotics given to healthy mice prevent inflammation. But Arthur wanted to know if probiotics could reverse inflammation and whether that would prevent cancer.
She set up a study that used mice genetically designed to develop colitis. At the first sign of inflammation, she fed them common probiotics. But something surprising happened: the probiotic mice developed cancerous tumors much earlier than the control group did.
“I was stunned,” Jobin says. “I thought the probiotics might offer a minimal benefit.”
Still, Jobin and Arthur are careful not to say that probiotics caused cancer.
“We think they changed the composition of the microbiota in the mice,” Arthur says. And that change ramped up cancer development.
But most of those genetically altered mice were going to form tumors anyway. The vast majority of people with colitis won’t get colon tumors. Still, altering a patient’s microbiota might have unforeseen consequences.
How do probiotics alter the gut? And how can we maximize the benefit and minimize the detriment?
Jobin says it might have to do with when you take probiotics. If you have mild digestive issues, probiotics might keep “bad” bacteria in check and that in turn could help alleviate symptoms. But once a person has a gastrointestinal disease that has triggered a strong immune response, probiotics may no longer provide a benefit and might fuel an already existing bacterial problem in the patient’s gut.
Those “maybes” and “mights” aren’t very scientific. What do those “good” bacteria” actually do once inside our bellies?
“We don’t know,” Jobin says. “We need to learn a lot more about probiotics and the microbiota.”
Christian Jobin is an associate professor in the Departments of Pharmacology, Medicine, and Microbiology and Immunology in the School of Medicine. Janelle Arthur is a postdoctoral fellow in Jobin’s lab. They and contributing colleagues received funding from several sources, including the National Institutes of Health, the American Institute for Cancer Research, and UNC’s University Cancer Research Fund.