A team of UNC researchers has discovered that populations of HIV strains differ between blood, which is the focus of most HIV research, and semen, the main point of HIV transmission.
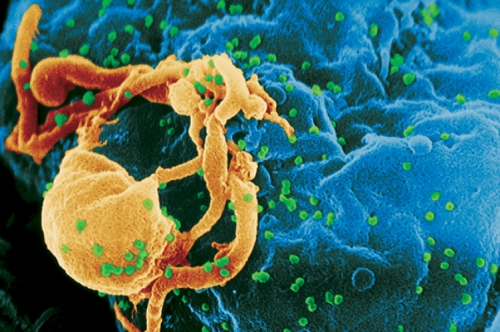
HIV is adept at evading the immune system because it mutates into many strains within one person’s body. By the time the immune system creates cells to target one strain, another strain is poised to multiply and take the target’s place. It’s a never-ending competition between the immune system and virus evolution.
The team, led by virologist Ron Swanstrom, looked at sixteen HIV-positive men and found three different ways that populations of the virus formed in their blood and semen.
In the first scenario, the virus was identical in the bloodstream—where HIV goes first after it enters the body—and in the seminal tract.
In the second scenario, say that the person’s blood contained strains A, B, and C in roughly equal amounts. In this scenario, the person’s semen also contained strains A, B, and C, but C was much more abundant. Swanstrom believes the virus underwent rapid replication but did not have enough time to evolve after it entered the seminal tract.
In the third scenario, the person’s semen contained strains D, E, and F, and not the A, B, and C strains found in the blood. The strains were different because the virus had replicated for a long time (months to years) after it entered the seminal tract, and it evolved as a separate population from the virus in the bloodstream.
To explain why HIV may be able to replicate in the seminal tract, Swanstrom’s team looked at immune signaling molecules—cytokines and chemokines—in semen. The team found that some of these molecules are at higher concentrations in HIV-infected men. HIV lives in immune cells, so the more cells that are recruited and activated by signaling molecules, the better the environment for HIV to replicate and evolve. The greater concentration of the signaling molecules in semen than in blood could explain how the target immune cells are attracted to the seminal tract, where they can support the different viral populations.
“Understanding how HIV establishes separate populations in the body will help us understand disease progression and pathogenesis,” Swanstrom says. “In this case, independent replication of the virus in the seminal tract can change the nature of the virus that is transmitted.”
Next, Swanstrom’s lab will focus on finding the properties of HIV that cause the differences in viral populations in blood and semen.
Noor White is a research technician in biology at UNC.
Ron Swanstrom is a professor of biochemistry and biophysics in the School of Medicine. His paper was published in PLoS Pathogens in August 2010. Participants in this study were from the Kamuzu Central Hospital, part of the UNC Project in Malawi, and from the CHAVI 001 Cohort in North Carolina.