Frank has been a medic in the army — Special Forces — for almost sixteen years. Sometimes, out in the middle of nowhere, in bad weather, or during gunfire, he has to keep critical patients alive for as long as seven hours before he can get them to a hospital and an operating table.
When a wounded soldier is bleeding internally, Frank has few options. “It comes down to simple hope that his body will heal itself,” he says.
On a recent tour in Afghanistan, Frank’s unit got ambushed. Thirteen casualties, five of them critical. A junior medic was working on an Afghan soldier with a front-to-back bullet hole in his stomach. “This guy’s going,” the junior medic called to Frank. They couldn’t find a pulse, but they could detect a faint heartbeat in his chest. They gave him a small amount of IV fluids. “We gave him five hundred CCs of Hespan, five hundred of normal saline — just enough to get his carotid pulse up,” Frank says. “If we raise the blood pressure any more, we’ll blow the internal clot off.” They maintained this patient, barely alive, for two hours. He eventually had surgery and survived. “That’s pure luck,” Frank says.
What if medics had a reliable tool to stop internal bleeding? What if that product kept, fresh and sterile, for years? What if they could just grab a pack of preserved platelets, insert a syringe of saline, then infuse it into their patients? And what if those preserved platelets stopped the bleeding quickly?
Tom Fischer, associate professor of pathology and laboratory medicine at UNC-Chapel Hill, and Arthur Bode, professor of pathology and laboratory medicine at East Carolina University, think that they have almost perfected such a product — lyophilized, or freeze-dried, blood platelets.
This technology got its start in the mid-1970s, when Marjorie Read, now professor emeritus of pathology and laboratory medicine at Carolina, was an assistant professor in the lab of Kenneth Brinkhous, a researcher and then-chair of pathology and laboratory medicine who would become legendary for his discoveries leading to a treatment for hemophilia.
Back in the seventies, Bode was also at Carolina, working for a few months as a technician in the pathology labs of Herbert Cooper and Robert Wagner. Soon Bode enrolled in graduate school at Carolina, and he got to know Read and Brinkhous well. “It was ingrained in my mind that this was a world-class platelet lab,” Bode says.
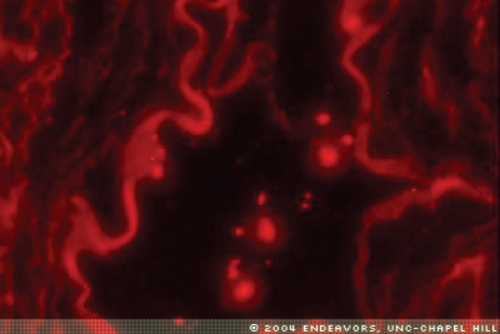
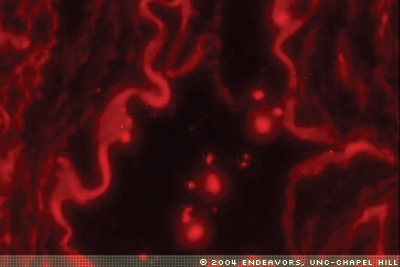
During that time Read began experimenting with ways to preserve the platelets she used in her everyday lab experiments. Scientists have traditionally used chemicals such as paraformaldehyde to “fix,” or preserve, cells for viewing under a microscope. That’s what Read was doing when she noticed that, even though the platelets had been fixed, they were still spreading over the glass, extending tiny “arms” called pseudopods. That’s what live platelets do when they activate. Inside your body, platelets circulate, waiting. When a blood vessel breaks, a platelet receives signals from several different enzymes in the blood. The platelet activates, releasing its internal stores of ATP and other chemicals. That release signals other platelets. They form a sort of “Band-Aid” — a rough plug of platelets, red blood cells, and fibrin that is the first step toward stopping bleeding.
So these fixed platelets were trying to form this plug on the glass slide. Read was surprised. “By traditional knowledge, fixing a cell means that you’ve killed it,” she says. A fixed cell was good for viewing under the microscope, but that was about it. But those spreading platelets made Read wonder. What if she fixed the platelets as usual, but cut back on the amount of paraformaldehyde? Maybe she could preserve the platelets while keeping them active enough to use in experiments, even in diagnostic tests.
She and Brinkhous decided to do just that. They found that, using just the right degree of fixation, they could preserve platelets with paraformaldehyde, but then, when they needed the platelets, they’d wash them, essentially reversing the fixation and ending up with active cells.
Read and others in the Brinkhous lab used this fixing method for a couple years to preserve platelets, including those used in a test Brinkhous developed to diagnose von Willebrand’s disease, a bleeding disorder. As they worked day to day, the researchers found that, even though they kept the fixed platelets in the refrigerator, sometimes the platelets would lose activity after a week or so. Read says, “Herb Cooper found that some of the platelets were growing certain bacteria, which inactivated specific receptors on the platelet surface. Then we were sitting around one afternoon, and we said, ‘Why the heck don’t we freeze them?’” So they did. Then they decided to dry the platelets as well, so they wouldn’t have to keep the platelets in the freezer.
“You sit around, and you say, ‘Why don’t we try this? Or why don’t we try that?’” Read says. “Some of these things work, and some of them don’t.” This one worked. In the early 1980s, Carolina patented the preservation and freeze-drying methods on behalf of Read and Brinkhous.
By 1988, Bode had become a faculty member at East Carolina, and he was working on chemical cocktails that would keep fresh platelets stable and active until they were needed. But then the Food and Drug Administration declared that platelets could be stored for only five days to avoid the risk of bacterial contamination. That meant that Bode’s extended-storage method wasn’t going to have any practical application. The U.S. Army stopped funding the work. Bode began looking for other funding, and he talked to Lynn Yaffe at the Office of Naval Research. Bode remembers Yaffe saying, “If you could just freeze-dry platelets, you could solve so many of our problems.”
“Immediately,” Bode says, “the image came back to my mind of Marjorie Read loading up the lyophilizer every Tuesday morning.” What if Read’s and Brinkhous’ freeze-drying method could work not just for platelets used in diagnostic tests but for those used to treat people? “I went rushing back to Chapel Hill,” Bode says. He and Read ended up putting together a proposal that was funded by the Office of Naval Research.
Then they worked together, perfecting the technique, for four years. Read says, “It was a matter of going through a number of different fixatives and trying them under different concentrations, times, and temperatures.” They worked to make the fixation much more gentle. “Taking water away from a cell and then adding it back quickly is a terrible challenge to the integrity of the cell itself,” Bode says. Most scientists would expect platelets that have been freeze-dried and rehydrated to end up a “leaky mess.”
But by 1992, Read and Bode hit on the perfect conditions for fixation. The end product was a fine white powder. But when they added saline to it and examined the rehydrated platelets under a microscope, they were hard to distinguish from fresh ones.
Bode and Read tested the preserved platelets in rats and dogs, and the platelets proved to be safe. More experiments, in dogs and pigs, show that the freeze-dried, rehydrated platelets work much better than fresh ones at stopping acute bleeding. Add saline or water, then administer by an IV, and the lyophilized platelets go to work. Freshly isolated platelets, for little-understood reasons, need about twelve hours in the body to become active. And, while fresh platelets lose their function and develop risk for bacterial contamination after only five days, these lyophilized platelets have been shown to work after being stored for up to five years.
In the mid 1990s, Carolina and ECU jointly patented the technology, and a company called Centeon licensed it. Centeon scientists discovered that the preservation and freeze-drying process adds another benefit — it sterilizes the platelets. Centeon scientists introduced eight different viruses, including HIV and hepatitis, into the platelet mix. During the preservation process, all eight viruses were killed. Carolina, ECU, and Centeon jointly patented the use of the process for sterilization.
In 2000, Read retired. Tom Fischer stepped in to help carry on the work.
In 2001, Centeon had problems with one of its other products, and for financial reasons had to pull out of the platelet project. Carolina reclaimed the license in 2001. Two years passed. With the help of Carolina’s Office of Technology Development, Fischer and Bode became convinced that if they were going to get these platelets into clinical trials, they’d have to start their own company. Fischer took a Carolina Kenan-Flagler Business School class intended to help faculty understand the business side of commercializing inventions. Through that class he met entrepreneur Stan Eskridge, who helped form their company, Hemocellular Therapeutics, which was founded in 2002. Eskridge is president, and Dana Fowlkes, a former Carolina pathology professor who has formed several businesses, serves as CEO.
Since then the researchers have spent more time evaluating the platelets. They aren’t sure exactly why the freeze-dried platelets work faster than fresh ones, but the scientists’ theory — one that they’ve published several journal articles supporting — is that it’s an accidental by-product of the preservation method, which includes the chemical paraformaldehyde. “The paraformaldehyde molecule has a reactive chemical group on each end of it,” Fischer says. “So it’s got two active parts, and it will sit down and join two proteins together on the surface of the platelet so that they are then stabilized,” he says. Bode and Read also used some of Bode’s previous work with fresh platelets to put the platelets in a responsive state before preservation. The platelets are, the researchers believe, primed for activation.
Another plus — the rehydrated platelets do their job, then get out quick. Once infused into the bloodstream, they go straight to the wound site. In animal studies, the platelets circulate in the body for about fifteen minutes before the spleen recognizes the paraformaldehyde as a foreign substance and disposes of the platelets. That’s enough time for them to pass by the wound site a hundred times, Fischer says. Enough time to activate the lifesaving first plug.
But because the spleen eliminates the freeze-dried platelets quickly, they don’t go on to cause the tighter bond of secondary hemostasis, as normal platelets might. That’s a good thing because secondary hemostasis, under certain conditions, can cause clots in blood vessels, which can lead to strokes or heart attacks.
Because the freeze-dried platelets don’t do complete secondary hemostasis, they are not a substitute for fresh platelets but a supplement, Read says. Before using whole blood or fresh platelets, which may go to waste if a patient continues to bleed, medical workers could use the freeze-dried platelets to quickly stop bleeding, and then, a few hours later, use fresh platelets or plasma to replenish blood loss.
After work that spans more than thirty years, the team is close to sending the freeze-dried platelets into human safety testing — one of the final steps in taking a treatment to market. “A best-case scenario,” Fischer says, “is that we’re going to be in the human clinic toward the very end of the year.”
Fischer is confident that they’ve got a viable product. But he and Bode still have more research ahead of them. Before the human safety testing, they must repeat some animal experiments using FDA specifications — larger groups of animals and more rigorous record keeping. And scientists at Hemocellular are creating a standardized process for manufacturing the platelets and for rehydrating them.
“We have spent a lot of time showing that the platelets work and understanding how they work,” Fischer says. “It’s time to go with it.”
Hemocellular Therapeutics is funded mostly by private capital. The Office of Naval Research funds Fischer’s lab to do some of the final studies required before the platelets can go into human safety testing. The Office of Technology Development is the only UNC-Chapel Hill office authorized to execute license agreements with companies. For more information on reporting inventions, contact OTD at (919) 966-3929 or visit http://research.unc.edu/otd/.