On a baseball field one hot summer evening in 1967, eleven-year-old George Plym watched a ball sailing toward him. As the moment approached to make the catch, he couldn’t make up his mind which ball to reach for — Plym saw two balls where there should have been one.
His parents took him to an eye doctor, who found nothing wrong with his eyes and prescribed rest. But Plym’s double vision worsened, and he started getting blinding headaches and bouts of nausea. A neurological exam confirmed his parents’ worst fears. A ball of brain tissue the size of an orange was pushing against Plym’s optic nerve. Plym’s neurologist diagnosed a grade-three oligodendroglioma — a late-stage, recurrent brain tumor.
When doctors diagnosed Plym’s first brain tumor, they thought he had about a year and a half left to live. Today, at age fifty-three, Plym is a retired sports-car technician who lives in Asheville, North Carolina. He has survived eleven relapses of his brain tumor, and he’s determined to fight his cancer to the death.
Most brain tumor patients are not as lucky as Plym. Many die within a year of being diagnosed with late-stage glioma. According to the National Cancer Institute, 20,500 people were newly diagnosed with a brain tumor in the United States in 2007. Of those, 12,740 died that same year.
Treatment for glioblastoma involves surgically removing the tumor and treating the area with a beam of radiation to kill tumor cells that the surgery missed. Chemotherapy follows for several weeks.
Radiation and chemotherapy keep Plym alive, although the treatment actually triggered some of his tumors. As Plym fights to stay alive, hearing loss, balance problems, seizures, headaches, numbness in his limbs, and double vision punctuate his day-to-day life. Radiation therapy has taken away his energy along with the tumor cells. “I would wake up feeling tired already, no matter how much rest I had,” Plym says. After each dose of radiation, he’s so tired that he can’t stay awake for more than two hours at a stretch. “That has continued over the years, and I’m still dealing with that,” Plym says.
Matthew Ewend treats hundreds of brain tumor cases every year at UNC Hospitals. Although the treatment works for some, it does not dramatically improve survival time, Ewend says. Most must endure the side effects of radiation and chemotherapy during the extra time the treatment allows them to live.
“It’s always difficult to tell a forty-five-year-old patient with grade-four glioma that the treatment might prolong their life by twelve to fifteen months,” Ewend says.
A major challenge of the therapy is targeting tumor cells with the radiation and chemotherapy, Ewend says. A specialized form of radiotherapy called brachytherapy delivers the radiation as close to the tumor as possible. In brachytherapy, radioactive seeds are surgically placed at the tumor site, or a catheter that delivers a radioactive liquid to the site is inserted into the brain. Ewend says brachytherapy cannot be performed on all patients and can cause brain swelling. The surgery involved increases the risk of a stroke, he adds, although surgery rarely causes one.
The biggest problem with current therapies is that the tumors almost always come back, Ewend says. About 90 percent of patients with high-grade glioblastomas die within eighteen months of therapy.
Ewend says that molecular therapies aimed at manipulating tumor cells to trigger their own death hold great promise. But there’s an obstacle — a membranous shield surrounds the brain and regulates the flow of molecules carried by blood into the brain. Ewend cautions that it would be no easy task to get a “magic bullet” treatment across the blood-brain barrier.
The question of how to treat brain tumors looms large, but the answer may lie hidden within the tumor cells themselves.
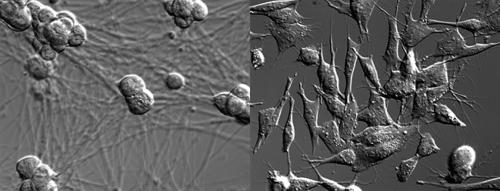
Mohanish Deshmukh, a neuroscientist at Carolina, is looking for answers inside the tumor cell. Deshmukh tried to exploit the innate vulnerability of brain tumor cells to a process called apoptosis. Cells in the brain, as everywhere else in the body, are programmed to die when the time is right. Age, stress, environmental agents, and microorganisms can turn on apoptosis, or programmed cell death, causing cells to die off and be replaced by new ones. Cancer can also trigger apoptosis.
“Apoptosis is an inherent mechanism of cell suicide that gets turned on when our cells detect abnormalities in themselves,” Deshmukh says. Tumor cells manage to override apoptosis before they go on an often fatal rampage, he adds. If they couldn’t override apoptosis, cancer would not be the scourge it is.
“This also makes many cancer cells resistant to death by chemotherapy because chemotherapy essentially tries to activate cell suicide,” Deshmukh says. Chemotherapy does not specifically target cancer cells and often fails because cancer cells override apoptosis while normal cells succumb to it. Doctors do a tricky balancing act when they decide just how much chemotherapy a patient can take. The holy grail of molecular oncology has been to find a way to target cancer cells for death without affecting normal cells, Deshmukh says.
Apoptosis destroys cells through a systematic, multi-step process. Traditional chemotherapy targets an early stage in apoptosis. A molecule called cytochrome c that occurs naturally in human cells targets a later stage of the process.
Deshmukh knew from previous research that several types of brain cells become resistant to apoptosis when they mature. Neurons need this resistance partly because they are difficult for the brain to replace and often must last until a person dies. Deshmukh’s team had found that normal neurons are sensitive to death by chemotherapy, but resistant to death by cytochrome c.
“For most normal cells, injecting cytochrome c means the game’s over. Not so for mature neurons. We were very surprised when we found out,” Deshmukh says. This difference between neurons and most other cell types is attributed to complex molecular cascades involving proteins that regulate cell division.
But the million-dollar question was whether brain tumor cells were also resistant to apoptosis by cytochrome c. Deshmukh sought to find out by testing cells from mouse models of two commonly occurring, late-stage brain tumors.
Deshmukh and his graduate student Yolanda Huang tested several different cell types from brain tumors and found that all were sensitive to cytochrome c. Around the same time, Sally Kornbluth, a Duke cell biologist who had been working on brain tumors and cell death, saw the same thing.
Kornbluth and Deshmukh joined forces. Kornbluth’s team implanted three types of human brain-tumor cells in mice, extracted the tumors and tested them for sensitivity to cytochrome c. All three tumors revealed the signature of cytochrome c-induced death, while normal human brain cells remained resistant.
To mimic human brain tumors more closely, the two teams asked whether cytochrome c could induce cell suicide in mouse models of glioblastoma and medulloblastoma. These mice had spontaneously formed brain tumors that closely resemble human brain tumors in their molecular characteristics. Once again, extracts from normal brain cells were resistant to cytochrome c, while those from the tumors showed distinct signs of cell death.
The results were rock-solid, and the researchers had indeed hit upon the Achilles’ heel of brain tumors. But a big part of the picture is still missing. Deshmukh does not know if cytochrome c can shrink tumors. All he has are molecular signatures of death in the tumors uncovered in a series of test-tube experiments.
“We don’t have a way of introducing cytochrome c into brain tumor cells,” Deshmukh says. Cytochrome c comes attached to a chemical structure called heme — the same chemical compound that colors blood hemoglobin red. Heme-attached cytochrome c protein is too bulky to get across the cell membrane.
“We’re screening for small molecule compounds that are cell-permeable and would have the same activity as heme-attached cytochrome c,” Deshmukh says. His team is also trying to modify cytochrome c to get it across the membrane. A third option may be to use nanoparticle technology to deliver cytochrome c to cells. The team is collaborating with Carolina nanotechnologist Joseph DeSimone to investigate that possibility.
Getting cytochrome c into tumor cells may not be Deshmukh’s only concern. Just getting the molecule into the brain — and only the brain — is a mighty challenge. Cytochrome c cannot be administered as an intravenous injection or taken as a pill because it targets actively dividing cells. The vast majority of normal neurons are non-dividing and therefore resistant to cytochrome c. But cells elsewhere in the body are in various stages of division, and just one systemic hit by cytochrome c could wreak havoc.
Eugene Johnson, a neuroscientist who works on neuronal apoptosis at Washington University in St. Louis, says that in principle, a small molecule that mimics cytochrome c could be administered by techniques such as convection-enhanced delivery to reach the bulk of the tumor and destroy it. “The difficulty is that I am not aware of any such compounds. But this may be an approachable problem,” he adds.
Deshmukh says he does not believe that a chemical compound would be ready for a first phase of clinical trials for at least another ten years.
Kornbluth says one possible application of the findings would be to use cytochrome c, engineered to permeate the cell membrane, instead of a chemotherapeutic agent in the wafers placed adjacent to brain tumors during the surgical removal of tumors. “This wouldn’t affect the normal brain cells because they’re not sensitive to cytochrome c,” she adds.
There’s promise in brain cancer research to slow the march of the disease one day. Until then, survivors pin much of their hope on the will to live.
“When I was young,” Plym says, “I had a big space between my teeth, and I was conscious of it. We thought about getting braces to get that straightened out, but the doctors said that I wouldn’t live long enough to have the braces off. Now, in my fortieth year of being a brain tumor survivor, I’m glad I went and got those braces. When I do die, I’ll die with a smile on my face.”
Prashant Nair is a master’s student in medical journalism at Carolina.
Matthew Ewend is the Chief of Neurosurgery and a Distinguished Associate Professor of Surgery. Mohanish Deshmukh is an associate professor of cell and developmental biology. George Plym is the founder and president of the Western North Carolina Brain Tumor Support Group.