Two years ago, Zhen Gu was a postdoc at MIT conjuring up an idea to change the way millions of people with diabetes treat their illness. Instead of daily injections, Gu thought, why not develop a way for patients to inject insulin once every week? What about once every two weeks? His inspiration was his grandmother.
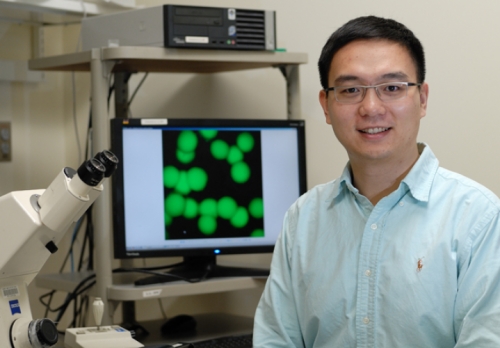
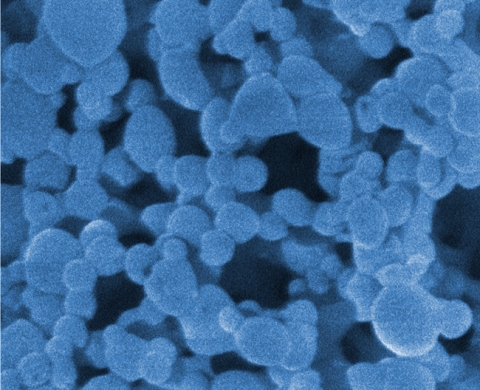
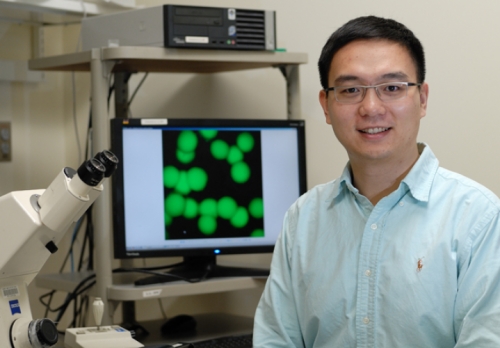
Courtesy of the Zhen Gu lab
Zhen Gu in his lab with a computational design of his nano-network.
Click to read photo caption. Courtesy of the Zhen Gu lab
“She was very old when her diabetes forced her to use daily injections,” Gu says. “I remember her telling me it was so painful, day after day. And sometimes she’d forget the injection.”
Gu, who came to UNC in 2011, told her about his new idea—inject a substance full of nanoparticles that release insulin over time so that daily injections become a thing of the past. “I remember her happiness when I told her,” Gu says.
Diabetes runs in his family, and though his grandmother knew she’d never reap the benefits of her grandson’s research, she knew that family members and millions of others might. And, as Gu says, maybe even cancer patients will benefit.
In people with type 1 or advanced type 2 diabetes, blood glucose levels rise to unsafe levels because the pancreas can’t secrete insulin properly. Over time, patients can develop chronic complications, such as blindness, kidney failure, seizures, unconsciousness, brain damage, heart disease, and limb amputation.

Wikimedia Commons
One of the first pens developed for insulin injections for diabetes patients.

Click to read photo caption. Wikimedia Commons
To keep glucose levels in check, patients must constantly monitor their blood sugar, often injecting themselves daily with specific and differing amounts of insulin. Drawing blood and administering shots can be painful. And the body’s ability to absorb insulin can change from day to day, making it difficult to figure out how much insulin to inject.
Gu’s response: create a sort of artificial pancreas—a closed-loop system, he calls it. “It would continuously and intelligently release insulin in response to rising glucose levels,” he says. But the artificial pancreas he had in mind wasn’t a clunky device. Other researchers are working on that and other ways to mimic the pancreas. Gu’s method is based on nanotechnology: he envisioned an injectable gel full of insulin-carrying nanoparticles that would regulate glucose over time.
It took two years, but his team has proven that it’s possible.
Gu and colleagues created nanoparticles made of glucose oxidase enzymes and a modified form of a substance called dextran.

Wikimedia Commons
Chitosan from shells of crustaceans, such as shrimp, can be commercialized and used for various purposes, including research such as Zhen Gu’s.

Click to read photo caption. Wikimedia Commons
The particles have solid cores of insulin. Some cores are coated with a positively charged material made of chitosan, which is naturally found in shrimp shells.

Wikimedia Commons
Seaweed is a good source of alginate, which companies commercialize for various uses, including research such as Zhen Gu’s.

Click to read photo caption. Wikimedia Commons
Other cores are coated with negatively charged material made of alginate, which is naturally found in seaweed.
As the nanoparticles are mixed together, the opposite charges attract, forming what Gu calls a nano-network. Due to that attraction, the nanoparticles stick together and are kept from dispersing throughout the body when injected under the skin. “But the blood sugar can penetrate into the nano-network through capillaries,” he says.
When that happens, the nanoparticle’s glucose oxidase enzymes convert the blood glucose into gluconic acid, which breaks down the modified dextran and penetrates the insulin cores. The insulin then decreases the amount of glucose in the blood. Meanwhile, the gluconic acid and dextran harmlessly dissolve in the body.
“We’ve tested the technology in mice,” Gu says. “One injection maintained normal blood sugar levels for up to 10 days.” It can last so long, he says, because not all of the nanoparticles are broken down immediately. Some break down and release insulin until glucose levels are lowered.

Courtesy of the Zhen Gu lab
The gel-like nano-network that is injected under the skin. When it comes in contact with high blood glucose levels, the substance breaks down and releases insulin to lower blood sugar for up to ten days.

Click to read photo caption. Courtesy of the Zhen Gu lab
But some particles stay intact. Then, when blood glucose rises again, more nanoparticles are broken down and more insulin is released.
His team is now perfecting the nanotechnology to use in larger research studies before seeking funding for clinical trials.
Gu’s research couldn’t spare his grandmother the pain and frustration of living with advanced type 2 diabetes; she died not long after he told her about his new approach. But if his nano-network holds together, we’ll have a better way to battle an often debilitating disease.