Two men. Both college students in the same North Carolina town.
Two isn’t a big number. But to a team of doctors and researchers fighting the spread of HIV, two was enormous.
These two men harbored “acute” HIV infections — infections so new that the standard HIV antibody test won’t detect them. Infections at their most contagious.
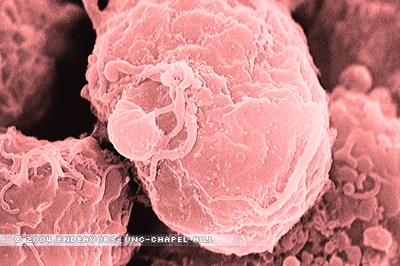
When HIV first invades, the body has not yet made antibodies to the virus. HIV begins replicating, and the victim might have a fever, a sore throat, and other flu-like symptoms.
One to three weeks after infection, the body creates antibodies to HIV. It is these antibodies, rather than the actual virus itself, that the standard test detects. Today that test is pretty sensitive, so it can detect more than 90 percent of infections within three to four weeks of transmission. But there is still that one- to three-week acute-infection period when HIV can hide.
So, using only standard testing, the HIV in these two college students wouldn’t have shown up. But in November 2002, the State of North Carolina and an aggressive group called the STAT (Screening and Tracing Active Transmission) team enlisted the help of the State Laboratory of Public Health to begin subjecting every blood sample tested for HIV to an additional test. A test that detects the RNA of the virus itself.
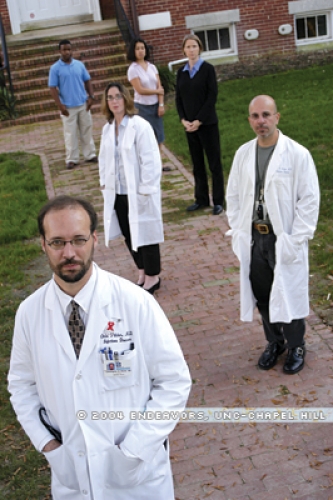
It was this RNA test that uncovered the acute infections in these two college students. And in February 2003, the STAT team — clinicians Chris Pilcher, Peter Leone, and Lisa Hightow, epidemiologist Pia MacDonald, and program coordinator Trang Nguyen — first heard about them. Each Friday the team gathers to listen to state disease-intervention specialists give summaries of every new case of acute HIV in North Carolina. They hear where the person lives, his or her age, a bit about the person’s lifestyle. They discuss what it might mean.
So, on that Friday in February, they heard about case one — male with an acute infection, a college student. Then, case two — also male, also an acute infection, also a college student. It was just two. But these researchers were alarmed.
Why? An acute HIV infection is not only hard to detect. It is, researchers believe, HIV at its most contagious. Studies show that during the acute stage, the viral load (the amount of virus in the blood and other bodily fluids) is at its highest. “Acute HIV is not just the time when the infection might be missed,” says Pilcher, assistant professor of medicine and leader of the STAT program. “It’s the moment of maximum public health threat. And given how unusual it is to detect a case during the acute period, each detected case of acute HIV infection has to be seen as the tip of a potential iceberg of active transmission in a community.”
So these two cases were serious. Out of five acute cases found in three months, two struck college students. Why?
The STAT team started brainstorming. No studies had suggested colleges as hot spots for transmission. Was this the start of a new trend? “Or maybe,” says Hightow, a fellow in infectious diseases, “this is what happens all the time, and we just didn’t know about it because we never really looked.”
The group needed to dig. In the past few years, how many more college students had turned up HIV positive? For the legwork, they looked to Hightow, the junior member of the team. So she prepared a questionnaire, and in April she started making trips to North Carolina’s Department of Health and Human Services (DHHS). Two or three days a week, she drove forty minutes to Raleigh and camped out in the DHHS break room for a half day. She read, one by one, the record of each person eighteen to thirty-five years old who was diagnosed with HIV in the three counties that make up North Carolina’s Triangle — Durham, Orange, and Wake. She limited her search to cases diagnosed between January 2000 and March 2003.
These were thorough records. North Carolina requires that hospitals, doctors, and health departments report every positive HIV test. Then a disease-intervention specialist contacts each patient and conducts a detailed interview. The specialist helps the person notify their sexual contacts and assists in finding care.
So, a lot of paper — 296 records in all. Whenever she found the record of a college student, Hightow recorded the answers to about twenty-five questions. Sex, age, zip code. Which college? Recreational drug user? Which drugs? Patron of dance clubs? Which ones? Sex with men? Sex with women? Sex with fellow college students? Sex with students at other colleges? Traveled outside North Carolina recently? Ever paid for sex? Ever met sex partners on the internet? It took Hightow six weeks.
She did indeed find a mini-outbreak of HIV — twenty-eight male college students in the Triangle infected with HIV in those three years. One female college student.
Even those twenty-eight cases might not sound like a big deal. But, Hightow says, if you look at HIV rates among the men at individual colleges, you’ll see the problem. At some schools, the incidence rate — the number of men with HIV compared to the total number of students, extrapolated for comparison — is about 200 per 100,000. The incidence rate for North Carolina men overall is only 27 or 28 per 100,000. “So when you look at it that way, some of the colleges have incidence rates that are similar to those in Africa,” Hightow says.
Why are these students getting HIV? Compared to other North Carolinians diagnosed with HIV in those three years, the college students were more likely to report certain characteristics. Most — 88 percent — were African American, and the same percentage reported having sex with other men. Just those factors could mean a higher HIV risk, says Leone, associate professor of medicine and medical director of the HIV prevention and care branch of the N.C. DHHS.“In the United States, people tend to have sex with someone like themselves. Young black men who have sex with men — that’s not a big pool of partners.” A smaller pool of partners means a higher risk of infection.
It’s only natural to speculate about other reasons. For instance, researchers are finding that some types of “inherited resistance” to HIV — such as a gene mutation that makes it harder for HIV to infect — are rare among African Americans. Leone says that biological differences certainly play a role in the increased rates of HIV in countries such as Africa. But, he says, this college-student epidemic is most likely the result of behavior and environment.
So, what are the behaviors that the newly diagnosed men had in common? Thirty-six percent reported having sex with both men and women. Using the drug ecstasy? Twenty-seven percent of the infected students. Meeting sex partners at gay dance clubs? Forty percent. And meeting sex partners on the Internet? Twenty percent.
These high-risk behaviors may be caused in part by the men’s reluctance to identify themselves as homosexual or bisexual, Leone says. At their initial testing, many of the men didn’t indicate that they had sex with men, but they revealed that during their interviews with disease-intervention specialists.
Those same anxieties may also make prevention efforts less effective. Especially in a tight-knit community such as a college, “If we’re having HIV testing in a certain place on a certain night, you may not want to stand in line to get tested,” Leone says. “Because if you do, people assume certain things about you.” These students might not respond to prevention messages aimed at, for instance, gay white men. “We don’t know how to tailor our prevention activities to be effective,” Leone says.
One change since this outbreak was reported — all twelve historically black colleges and universities in North Carolina are planning to offer free, confidential HIV testing for the first time. Leone says that the STAT team is working on prevention efforts with student-health officials at all the colleges in the Triangle.
Leone believes that people shouldn’t have to single themselves out just to get an HIV test. “HIV testing should be a routine part of health care,” he says. “We shouldn’t depend on you identifying yourself as a person at risk, or on your provider asking the right questions and suggesting a test.” This year the Centers for Disease Control has launched an “Advancing HIV Prevention” initiative that includes making HIV testing part of routine medical care and testing people outside of traditional medical settings.
Since the STAT team’s initial study of the college-student outbreak, which Hightow presented at the 2003 National HIV Prevention Conference, the researchers have looked farther. “The patients were saying that they were sleeping with other students outside the Triangle area,” Hightow says. “We thought we needed to expand this and see what was going on throughout the entire state.” So Hightow, this time with help from some medical students, went through records from thirty-one more counties — those with a college nearby. The researchers found additional N.C. college students with HIV, bringing the total to fifty-six cases.
Then Evelyn Foust of the N.C. DHHS called on the CDC. In August 2003, eight “disease detectives” from the CDC’s Epidemic Intelligence Service arrived in North Carolina. They spent about two months interviewing fifteen of the newly diagnosed young men. They also interviewed two HIV-negative men of similar age and race. They wanted to find out what was different about those who haven’t gotten infected.
“These aren’t the only sexually active college students,” Leone says. “Why they got infected when others didn’t is something we need to understand.”
Newly returned from North Carolina, the CDC team is evaluating its results. Lisa Fitzpatrick, a medical epidemiologist with the CDC and leader of the team that visited North Carolina, says that though the new cases in North Carolina appeared largely among men, the CDC is concerned about the spread of HIV in this age group in general. “It’s important for people to realize that this is about young people — whether male or female — putting themselves at risk,” Fitzpatrick says.
The Carolina team echoes that thought. They believe that the outbreak they uncovered is likely a sign of a growing risk among young people in general. They decline to name the colleges involved. Were any of the newly diagnosed students at UNC-Chapel Hill? They won’t say. “There’s no reason to think that this is unique to any particular college, or even to North Carolina,” Hightow says.
Some statistics back up that position. In the first six months of 2003, the number of HIV cases diagnosed among men and women aged eighteen to twenty-five increased 23 percent in North Carolina, Leone says. Nationwide, it has been estimated that at least half of all new HIV infections are among people under twenty-five. And CDC statistics show that, among twenty-five states that report HIV-testing results, new HIV infections among homosexual and bisexual men have increased for the past three years.
“It’s obvious that what we’ve been doing isn’t working,” Leone says. “It’s a little too easy to say, ‘Well, just don’t have sex.’ Life is a lot more complicated than that.”
Collaborators on the research are Hightow, Leone, Pilcher, Pia MacDonald (assistant research professor in the Department of Epidemiology in the School of Public Health and project director of the N.C. Center for Public Health Preparedness), Andrew Kaplan (associate professor in the Departments of Medicine and Microbiology and Immunology),Trang Nguyen (project coordinator for the STAT program and a doctoral student in the Department of Epidemiology), and Evelyn Foust (head of the HIV/STD Prevention and Care Branch in the N.C. Department of Health and Human Services).