The young hemophiliac lay feverish in a UNC Hospital bed, his glands the size of baseballs. His body was deteriorating. Tests for cancer were negative, and as he worsened, doctors suspected a new mysterious illness. Hematologists Harold Roberts and Gil White sent a lymph node to Robert Gallo, who was studying retroviruses. In that sample Gallo found the HTVL III virus, and, along with other scientists, including White, wrote the first paper about HIV/AIDS to appear in the journal Science.
Back home at UNC’s Center for Infectious Diseases, Myron Cohen watched that hemophiliac die — the first AIDS death at UNC. That was 1982. Within months the hospital’s thirty-bed AIDS ward was filled to capacity. Many of Carolina’s hemophiliacs died before scientists learned in 1985 that heating blood products killed the virus.
“It was unbelievable,” Cohen says. “Our nurses watched patients die every week.”
Scientists searched for a cure, and in 1984 the federal government vowed to have a vaccine ready for testing in two years. Other scientists worked on treatments, and today there are more than twenty antiviral drugs that Cohen says have helped doctors turn HIV into a manageable disease. Still, forty thousand Americans are infected each year, and therapies, which many patients worldwide don’t have access to, are far from perfect.
So what happened to that vaccine? Why don’t scientists talk about curing AIDS anymore?
Playing with fire
Scientists initially thought that they could quickly develop a vaccine because vaccines for polio, smallpox, and hepatitis B were so successful.
“But we didn’t take into account the unique nature of HIV,” says microbiologist Bob Johnston, who is developing an HIV vaccine at Carolina.
Unlike other viruses, HIV knocks out the body’s ability to produce an immune response. So the body doesn’t even recognize the virus as an intruder for weeks.
Also, as Cohen points out, the virus mutates when the body does recognize it.
“So think about this,” he says. “We put an antibody in front of it. The antibody kills a few particles in the swarm. But the virus replicates as quick as it can, throwing off mutants at a very high rate — higher than many other viruses. That’s a big advantage it has.”
Still, researchers tried to make a vaccine like the one for hepatitis B. They took a protein from the outer coating of the virus and genetically engineered the protein’s gene into cells, then grew the cells in culture and purified the protein from them. This worked for hepatitis but not for HIV.
“The HIV protein induced immune responses,” Johnston says. But the neutralizing antibodies that could fight the virus weren’t activated. “So the vaccine didn’t stop the virus at all.”
Scientists also considered the Salk polio vaccine model, in which either heat or chemicals render the virus harmless. The body recognizes the vaccine and builds immunity. But Cohen says that scientists don’t completely understand how that virology works.
“Most of the vaccines for other diseases somehow mystically provide enough immunity so that you either never get infected or the infection is aborted so you never become ill,” Cohen says. “But we clearly don’t know how to do this for HIV.”
An attenuated HIV vaccine modeled after the Sabin polio vaccine would also be too dangerous. The Sabin vaccine is made from live mutant viruses, but they’ve caused polio in rare cases. Since HIV mutates as a part of its natural behavior, that’s too risky.
“I’ve come to think of HIV as evil,” Johnston says. “I’m assigning it adjectives that a scientist probably shouldn’t assign to such an organism. But whatever we do, it seems to have already thought of a response — so far.”
Johnston and others are now concentrating on vectored vaccines — putting genes that provide immunization against HIV into a different benign virus. Once inside the body, the immune system recognizes the HIV protein that’s expressed by the vectored virus — the vaccine — and builds immunity.
“There’s some hope for vectors,” says Johnston, “but none have made it to phase three trials. In primates, these vaccines have induced an immune response to the disease but they fail to protect against infection. The primates have the virus but the viral load is low. Their immune response suppresses the replication of the virus enough so that they don’t have overt disease.” The animals, though, get sick when exposed to a slightly altered version of the virus.
Johnston is trying to get around these problems by making a vectored vaccine particle that looks like HIV so the body creates antibodies strong enough to fight off actual infection. The vaccine replication occurs in the cell’s cytoplasm through an RNA intermediate — not DNA like HIV — so the host cell is destroyed rather than being persistently infected.
“The virus will replicate like an acute infection with no persistence,” he says. “We think that will make it safe.”
For this work, Johnston received two grants totaling $2.5 million from the International AIDS Vaccine Initiative, which receives funds from the Bill & Melinda Gates Foundation.
Johnston’s team also received a $5.2 million grant last fall from the National Institutes of Health for developing an adjuvant — an agent designed to turn on multiple cell signals so that the immune system response is stronger and triggered faster. In essence, Johnston says, the adjuvant boosts a vaccine’s intensity. So far, it has worked in mice that were exposed to the adjuvant plus flu vaccine. The grant funds primate trials.
The push for a successful vectored vaccine gained momentum after Science writer Jon Cohen wrote a book called Shots in the Dark: The Wayward Search for an AIDS Vaccine in 2001. Cohen wrote that we need a “March of Dollars” effort in vaccine research. Last year the Gates Foundation gave $287 million to vaccine research, and in 2005 the National Institutes of Health created the Center for HIV/AIDS Vaccine Immunology (CHAVI), spearheaded by Barton Haynes at Duke. It’s a $300 million worldwide effort that includes Myron Cohen’s UNC team. He’s one of six CHAVI core leaders.
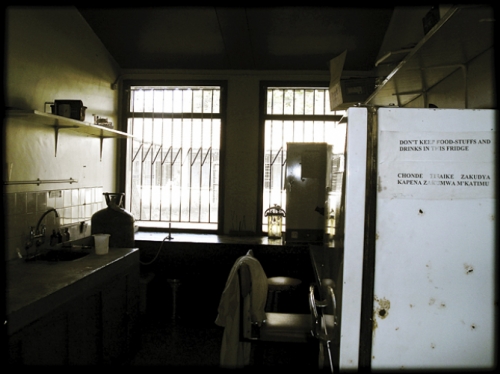
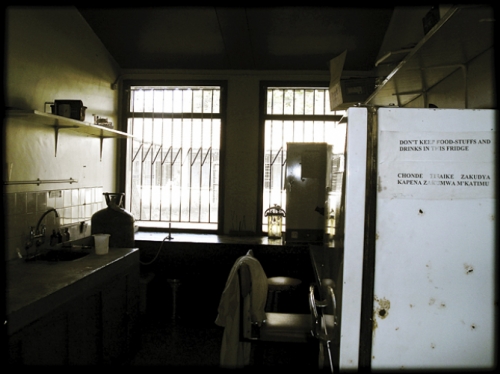
Photo by Susan Fiscus, ©2007 Endeavors magazine.
The Kamuzu Central Hospital Labs in Lilongwe, Malawi, where researchers log data as part of UNC’s effort to process samples for HIV research.

Click to read photo caption. Photo by Susan Fiscus, ©2007 Endeavors magazine.
As part of CHAVI, Carolina clinicians and microbiologists led by Cohen, Joe Eron, and Susan Fiscus gather and process blood samples and mucosal secretions from people who had been infected just days before getting tested for HIV. Finding such people is a tedious task that involves an RNA test to detect acute infection, which the typical HIV antibody test can’t do. Then the UNC team tries to enroll patients in research studies in North Carolina and certain African countries so that other CHAVI scientists can determine how HIV is transmitted and how it evolves. For instance, Carolina virologist Ron Swanstrom is trying to figure out if sexually transmitted particles are randomly selected from a patient’s virus population or if these particles have special characteristics that allow them to be transmitted.
“If there are special properties of that virus envelope protein,” he says, “then we would want to know that the antibody response we’re generating in a vaccine works against those properties.”
So the clarion call for an HIV vaccine has gone out. But there’s no such trumpet blast for curing AIDS.
Hope versus false hope
In the late 1990s, highly active antiretroviral therapy worked so well that scientists thought that HIV could be completely eradicated from patients in a few years, essentially curing the disease. But then doctors found that the virus hides in reservoirs where it doesn’t express the genes that drugs target, making AIDS seemingly impossible to cure. Since then, very few journal articles have even mentioned the word cure, and most scientists don’t even talk about it, Cohen says.
“Because these researchers are powerful, vocal, and articulate, they kind of walled off the idea that a cure is possible,” Cohen says. “Younger investigators have been afraid to touch the idea for fear of criticism, humiliation, and maybe even of being called stupid. To my knowledge there are no grants for curing AIDS. There are only grants for researching what’s called persistent latency.”
David Margolis, also a CHAVI researcher, has one of those grants.
Latency means that HIV infects the cell but doesn’t kill or damage it. The virus just sits there as genetic information that persists for a long time.
Margolis says, “This is probably the major reason why we can’t eradicate HIV infection with current therapies, which only target active enzymes, not the genetic information of the virus.”
A latent cell’s chromatin — the stuff around which DNA is wrapped — is closed, he says. That’s one reason why the virus’s genes are unexpressed. Margolis found that the natural enzyme histone deacetylase helps keep chromatin closed, but valproic acid curbs that enzyme’s production. So Margolis thought that if valproic acid could help open the chromatin, maybe the virus would be forced out of latency.
In a preliminary study, Margolis intensified drug therapy for four long-term HIV patients and then prescribed valproic acid. All patients saw a decline in latency, and three of four saw a statistically significant reduction of latent infection. Next, Margolis gave valproic acid to six patients but didn’t boost therapy. Three of six patients showed a significant depletion of latent infection; one patient’s decline was not significant; and the other two saw no drop.
These are the first experiments to indicate that breaking latency is possible.
Margolis says, “We’ll try to do our job to figure out how to get the virus out of latency, and the rest of the field will continue to make better and more potent antiviral therapy. Someday we’ll be able to put them together in a treatment, sort of like cancer therapy, to eradicate infection.
“We don’t imagine that this is ever going to be, ‘take a dose of penicillin and you’ll be fine.’”
Other problems will pop up, he says. For instance, a 2006 study at Case Western Reserve University showed that a patient’s viral load is not the only factor in determining how HIV affects the immune system. Viral load is measured in blood. But Margolis says that HIV is probably in tissue too, and we can’t measure that right now.
Because developing a cure will either never happen or take a very long time, Margolis and Cohen say, most scientists don’t want discussions about cures to give patients false hope.
Margolis also says that some scientists fear that people will take AIDS less seriously if researchers push the idea that curing AIDS is possible.
“Quite frankly, people already do that,” Margolis says. “In a lot of people’s minds, AIDS is already a problem that’s taken care of by medicine, or that happens in other countries to other people.”
But that mind-set doesn’t jibe with reality. For instance, medication doesn’t work for everyone, and about half of patients who’ve been on long-term medication have serious side effects such as nausea, dizziness, nerve pain, bone thinning, severe tissue loss, liver damage, and diabetes. Because of this, volunteers lined up quickly when Margolis wanted to study the effects of stopping medication. His findings show that HIV persisted and then replicated. Some patients had to go back on medication within two years because their immune systems could not control HIV.
Reducing replication

Photo by Jason Smith, ©2007 Endeavors magazine.
Bottles full of natural substances line the walls at Carolina’s Natural Products Research Laboratories. One of them holds birch tree bark, which contains betulinic acid — a potential curative agent for HIV.

Click to read photo caption. Photo by Jason Smith, ©2007 Endeavors magazine.
Margolis is the first to admit that patients desperately need less toxic therapy. K.H. Lee’s Natural Products Research Laboratories here at Carolina may have found one — in the bark of a birch tree.
Lee’s team screens thousands of natural compounds to see if any hold curative ingredients. In the case of HIV, that means finding herbs that naturally disrupt virus replication. Lee found that the Taiwanese herb Syzigium claviflorum contains betulinic acid, which slightly hinders HIV replication. Knowing that betulinic acid is plentiful in North American birch trees, Lee’s lab began a series of experiments to modify the betulinic acid’s chemical structure, in effect amplifying its natural tendency to suppress virus replication.
It worked. The medication blocks HIV’s ability to form its outer protein layer — the last stage of replication. This type of maturation disruption is a completely novel thing in HIV therapy. Currently, all HIV drugs except one stifle viral enzymes needed to complete DNA replication and make functional viral proteins. The other drug blocks HIV from fusing with the host target cell altogether. Because HIV mutates and builds resistance to these therapeutic approaches, Lee’s drug — bevirimat — could add another layer of defense while helping patients avoid severe side effects. It’s passed several trials and could be on the market in two or three years.
Lee says that better treatments are like vital pieces to a puzzle that’s far from complete. And there’s a chance it may never be fully solved.
Everyone would like one solution to AIDS, but Margolis says that’s not going to happen.
“There’s not one answer to cancer or heart disease or poverty,” he says. “So we need treatment, we need a vaccine, we need a cure, and we need prevention.”
And even if we eventually stop the epidemic, HIV won’t go away.
“All you need to cure syphilis is one dose of penicillin,” Margolis says. “And do we still have cases of syphilis? Yes we do.”