Bacteria are pretty simple. They have no secret compartments. They’re just tiny bags of stuff, mostly chromosomal DNA and plasmids. Chromosomal DNA is necessary for bacteria to live. Plasmids are not. They’re simply long, circular coils of DNA that broke free from the chromosome at some point in the bacteria’s evolution. But plasmids carry genes that can encode for such traits as antibiotic resistance. They can also replicate and donate themselves — and their resistance — to other bacteria.
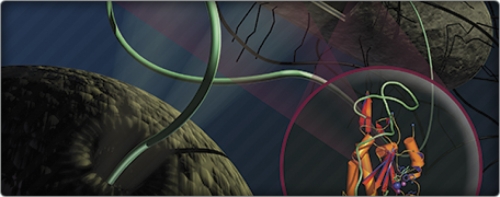
Plasmids are copied and carried to other cells by a mechanism called conjugation. (Imagine sharing a stick of braided licorice: grab a strand, tear it apart from the rest, and give it to a friend.) DNA has two double-helix strands — one called Watson, the other Crick (they’re named for the scientists who first described them).
To conjugate, the E. coli bacterium uses three enzymes. First a relaxase grabs onto Watson and breaks it. Next, while the relaxase is still holding on, a helicase unravels Watson from Crick. A replisome bursts in while the strand is unwinding; it shadows and copies Watson, replacing it with an entirely new one.
After the helicase has gone around one complete circle of the plasmid’s coil, the relaxase lets go of Watson, setting it free into another bacterial cell. Once there, Watson is replicated and reunited with his old friend Crick once again.
And if Watson had antibiotic resistance, now the new cell has it, too.
Steve Matson has been studying bacterial conjugation in E. coli since the early 1980s, when Matt Redinbo was still in high school. Matson decided to study TraI, which scientists had identified as a helicase — the enzyme responsible for unraveling the plasmid. But in 1991 Matson and his lab found that TraI was a lot more talented than anyone thought. It carries both the helicase and the relaxase — something that had never been seen before. TraI has all the tools to grab, unwind, and release a strand into a new cell.
Matson now had even more questions to answer, but he wasn’t intimidated. He wanted to learn more about the relaxase. But even after he isolated and purified the relaxase portion of TraI, he couldn’t see how it worked. He sought out Matt Redinbo, now a biochemist with a track record for crystallizing complex proteins (essentially taking a still photo on an atomic level).
But getting a good picture of the relaxase wasn’t easy. It took Redinbo’s team three years to get the shot. And just a few months before they got it, a group in Baltimore got it first — a glamour shot of the enzyme all alone, primped for its moment in the spotlight.
But while getting a snapshot of an enzyme by itself is good, catching it in the act is even better. Scott Lujan, a graduate student in Redinbo’s lab, crystallized the relaxase doing its business with DNA, which finally allowed the chemists to understand how TraI grabs and releases a single strand of plasmid DNA.
After decades of learning how TraI works, Matson and Redinbo wanted to figure out how to stop it.
Knowing that conjugation in E. coli is dependent on a well-functioning relaxase, the biochemists believed they could inhibit conjugation — and thus the transfer of antibiotic resistance — by making the relaxase bind with something that merely resembled the plasmid. DNA’s strands — Watson and Crick — are made up of sugars and phosphates. Bisphosphonates are molecules that are made up of two phosphates. Lujan used the simplest bisphosphonate he could find, hoping to confuse TraI so that it couldn’t interact correctly with the plasmid.
And it worked. It worked so well that the E. coli donor cells died before they could even attempt to share their goods with anyone else.
The results were so surprising, Lujan says, that he “actually did that first experiment eight times.” But when they brought in other bisphosphonates, including two simple drugs already on the market for osteoporosis, they saw similar effects. “We finally convinced ourselves that it was real,” Lujan says.
Redinbo and Lujan think that the cells die after the relaxase tears apart the two strands and the helicase starts to unwind them. The bisphosphonate prevents the relaxase from letting go of the unwound strand. Instead, Lujan says, “it just keeps unwinding and unwinding around and around, until it uses up all of the cell’s resources.” The cell dies, leaving behind only pieces of Watson and Crick.
But Matson and Redinbo only studied this relaxase inhibition in E. coli bacteria — which despite their reputation, are relatively benign: right now, there are billions of them in your lower intestine. The E. coli F plasmid, Lujan says, “was the first one ever discovered, so it’s been the most intensely studied and made a good model system.” Now Redinbo’s lab is certified to bring in nastier, meaner bugs to test: harmful bacteria such as Pseudomonas and Staphylococcus, which often have plasmids that encode for antibiotic resistance. As of now the team’s bisphosphonates don’t appear to be picky about the plasmids they work with — and when it comes to killing antibiotic-resistant bacteria, that’s a good thing.
Multi-drug resistant infections such as MRSA — a kind of staph bacteria that’s resistant to the antibiotic methicillin — are, ironically, most often picked up at the hospital. Redinbo foresees his team’s inexpensive bisphosphonates being a first line of defense against these infections. “If you’re going in for standard surgery,” he says, “and somebody on the ward has a resistant infection, you could give this as a preventive medication, especially for the elderly or young.”
And for patients who are already sick, Lujan says, the worst thing you can do is loosely dispense more antibiotics. Instead he envisions bisphosphonates used in hospitals to treat resistant infections prior to antibiotics.
“One thing to understand is that none of the bisphosphonates are particularly good antibiotics,” Lujan says. “A good antibiotic will wipe out 99.999 percent of the bacterial population. The best we’ve been able to do is 99 percent.”
So instead of trying to kill all of the bacteria in one fell swoop with an antibiotic, inevitably leaving resistant stragglers behind, Lujan suggests fighting bacteria with a one-two punch: hospitals could first administer bisphosphonates to an infected patient, wiping out the cells containing antibiotic-resistant plasmids. Once those cells are all dead — the team has seen this in as little time as an hour and a half — doctors could then hit the patient with a standard antibiotic, which should effectively kill off the rest of the bacteria.
But even if it doesn’t, at least the few left won’t have any resistance to give away.
Danielle Jacobs was a student who formerly contributed to Endeavors.
Steven Matson is a professor in and chair of the Department of Biology. Matthew Redinbo is a professor in the Departments of Chemistry, Biochemistry, and Biophysics, and a member of UNC’s Lineberger Comprehensive Cancer Center. Scott Lujan is a post-doctoral fellow studying biochemistry in the School of Medicine.