A blood brother
We’re closer than ever to creating synthetic blood cells that really work.
Scientists predict there will be a shortage of as much as four million units of donor blood in the United States by 2030. And although researchers have been trying for years, no one has ever managed to develop and manufacture a substitute for blood, says chemist Joe DeSimone. But he and his research team are getting close.
Natural red blood cells are flexible and can contort themselves to pass through all the blood vessels and microscopic channels throughout our bodies. The cells stay in circulation for about a hundred and twenty days, carrying oxygen from our lungs to various tissues and organs, before the cells wear out and our spleens remove them. The synthetic red blood cells scientists have created over the years are far too rigid to squeeze through the same tiny openings, DeSimone says. Imitation particles are always quickly filtered out of circulation by one organ or another.
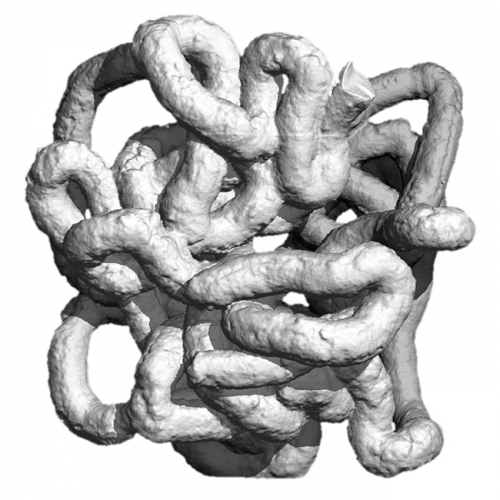
Now DeSimone and his colleagues have created a particle that’s not only the same size and shape as real red blood cells, but also has the same flexibility. And it can stay in circulation up to thirty times longer than the synthetic red blood cells of the past.
“PolyHeme and other synthetic blood products carry oxygen, but they don’t work just like real blood,” says Tim Merkel, DeSimone’s graduate student and lead author of their study. “This is why they haven’t been approved by the FDA. These products have taken and modified hemoglobin so that it’s not toxic and isn’t cleared from circulation too quickly. But in doing so, they changed the way that hemoglobin binds and releases oxygen and other gasses in the blood. This actually made the synthetic more dangerous for patients who had lost blood than simply administering saline, which replaces lost blood volume but doesn’t carry oxygen. Our approach has been to mimic the red blood cell as a whole to replicate its behavior in circulation.”
The research team used a powerful nanomolding technique, which was developed in DeSimone’s lab at UNC, to create disk-shaped molds for the particles (the same shape as true red blood cells). Then they filled the molds with a hydrogel solution and experimented with nanoparticles in various degrees of stiffness. Each nanoparticle was only six micrometers in diameter—one-fifteenth the diameter of a human hair.
When DeSimone’s team tested the particles in mice, the more-rigid imitation cells were filtered out of circulation within hours. Some worked their way as far as the lungs before they got stuck. The more-flexible ones, though, made it all the way to the spleen, the same place real red blood cells end up.
A truly functional synthetic blood would not only solve all our blood shortages, DeSimone says, it could also be a game-changer for the future of nanomedicine. If we could create particles that act the way red blood cells do—could go where they go, carry things the way they carry oxygen—these particles could be loaded with disease-fighting medicines and set loose to transport them throughout patients’ bodies. We’re not there yet—the new particles can’t carry oxygen, and they don’t stay in circulation for quite as long as real red blood cells.
“One of our next steps will be to carry oxygen with these or similar particles,” Merkel says. He and DeSimone want them to carry hemoglobin in its natural, unmodified form, along with other proteins and enzymes found in true red blood cells. If the particles could do that, Merkel says, they would be even more like the real thing.
Close to the bone
Synthetic bone material could turn dental implants into a one-day affair.
If you’ve ever had a tooth knocked out or lost one to decay, you might have had to endure a dental implant. These can take months—or even over a year—to complete. But Ching-Chang Ko wants to use his new biomaterials to make dental implant surgeries faster and less painful. “We could shrink it from a year to a one-day procedure,” he says.
Dental implants are necessary for all kinds of reasons—failed root canals, gum disease, congenital defects, wear and tear. The main reason the implants take so long, Ko says, is that they’re always cementless. Most other prostheses, including knee and hip replacements, use petroleum-based cements to stabilize the implants. Cement can’t be used in any kind of facial procedures, Ko says, because the residue may be toxic to the brain, the nerves in teeth, or the sinus cavity.
Here’s how dental implants work: first, the doctor makes a surgical incision in the patient’s gums where the tooth used to be and uses a series of larger and larger drills to make a hole in the underlying bone. Then the doctor inserts the implant—usually a screw made out of titanium—and stitches the patient’s gums up over it to keep them from growing into the hole over the next three to six months. (That’s about how long it’ll take the patient to heal.) Then it’s back to the doctor, who uncovers the implant and builds a temporary crown onto it to sculpt the gums into the right shape. Then more time for healing.
“Before you can put the permanent crown on, some people have to wait months, a year—sometimes more,” Ko says. But it’s definitely better than leaving the toothless space empty. If nothing replaces the lost tooth, Ko says, the bone beneath it will atrophy and shrink over time, weakening the jaws. Eventually you might have a hard time chewing at all, Ko says. An implant can replace the tooth and help keep the jawbone strong by giving tissue a structure to grow around.
Ten years ago, when the field of tissue engineering was just getting off the ground, Ko had already spent years studying how natural bone generates, degenerates, and remodels itself over time. And he’d seen scientific papers that described how apatite, a phosphate mineral and major element in natural bone, could be crystallized and made bone-like in the lab. But scientists have never been able to make materials strong enough to work. Even now, most researchers in the bone tissue engineering field focus on polymers, Ko says, which aren’t as strong as bones are. So Ko started creating and testing substances made from apatite, collagen, and other materials found in natural bones. He wanted to engineer a tissue that mimicked real bone and could actually take part in the generating and remodeling processes.
In 2009 Ko and Duke business professor Jon Fjeld founded Ironwood Material Science, Inc. based on the biomaterials Ko developed, called biomimetic nanocomposites. These could become the first effective synthetic bone materials, Ko says. His bone cement, Gemosil, has already been shown to work in small mammals. But the real challenge will be to make it work in larger animals, namely humans. Eventually, he hopes to prove it safe for dental and craniofacial implants.
“This material mimics the nature of bone ingredients,” he says. The two main ingredients are hydroxide and gelatin—both of which are found in natural bone. When Gemosil is used on an implant in the lab, the real bone that surrounds the stem of the implant recognizes the cement’s composition and grows into the new porous surface, locking the two together. “It’s almost like the natural remodeling process,” Ko says.
The Synthnode
Could an artificial, injectable lymph node teach your body how to identify pathogens?
Carla Hand and Steve Meshnick have created a tool that could revolutionize vaccines: a synthetic lymph node. Their device, called the Synthnode, has the potential to help develop new vaccines, make current ones more effective, and bring rare vaccines to more of the people who need them most.
Antigens—foreign bits of viruses, bacteria, and parasites—are what trigger the body’s immune response. The antigens are shuttled out of circulation and into lymph nodes, where they’re destroyed. But first the antigens are used to educate immune cells on what invaders look like. Vaccines take advantage of this immune cell “learning” by introducing an antigen so the immune system will recognize it if it shows up again. But sometimes it’s difficult to stimulate an immune response to the antigen of interest. Enter the Synthnode.
The Synthnode is roughly the width of a matchstick, and half the length. It can be loaded with a vaccine or a combination of vaccines and injected under the skin, where it degrades after one month. Structurally, it’s similar to a 3 Muskeeters bar with microscopic holes punched in the chocolate. The spongy yet dense inner layer stores tiny antigen bits where they can be accessed by larger immune cells, but can’t get out into circulation. The porous outer layer allows immune cells the freedom to enter and exit, just as they do with real lymph nodes. The difference is that the preloaded antigen hasn’t been diluted by circulating around the body. And it’s stuck in one place, so more immune cells learn what it looks like, leading to a more robust immune response.
Many vaccines that have been proven effective for use in animals aren’t available for use in humans. In animal vaccines, an adjuvant is included to create a stronger immune response and stronger future immunity. Unfortunately, adjuvants can have severe side effects, so they aren’t used in human vaccines. Here the Synthnode can help as well. In trials the tool has already proven to be more effective than some animal adjuvants, and it’s safe for human use. The Synthnode is so good at provoking an immune system response that it doesn’t have to use as much antigen as a vaccine normally does. This means that vaccines that are rare or expensive could be stretched to immunize more people.
Hand and Meshnick won a Grand Challenges Explorations grant to fund their research, and they will conduct preclinical trials with other recipients of Gates Foundation grants. They hope their invention will help to combat the spread of infectious diseases, especially malaria and dengue fever. “No vaccines exist for these diseases now,” Hand says. “We hope that the Synthnode may make development of these vaccines easier.”
Noor White is a research technician in biology at UNC.
Timothy Merkel is a graduate student in the Department of Chemistry. Joseph DeSimone is the Chancellor’s Eminent Professor of Chemistry in the College of Arts and Sciences and in the Institute for Advanced Materials, Nanoscience and Technology. Their synthetic blood study was published in Proceedings of the National Academy of Sciences in January 2011. The team used PRINT (Particle Replication in Non-wetting Templates) technology to create the nanoparticle molds. Their work was funded by an American Recovery and Reinvestment Act stimulus grant from the National Heart, Lung and Blood Institute.
Ching-Chang Ko is an associate professor of orthodontics in the School of Dentistry. His work is funded by the National Institutes of Health, the North Carolina Biotechnology Center, and Carolina KickStart.
Carla Hand is an assistant professor and Steve Meshnick is a professor, both in the Department of Epidemiology in the Gillings School of Global Public Health.