In April, 57 people at a nursing home in Chatham County tested positive for COVID-19. That number includes both residents and staff members. That same month, 74 Mountaire Farms employees also tested positive — that’s more than one-fifth of the chicken plant’s workers.
People are quick to associate the virus with major metropolitan areas hit hard in the early months of the pandemic. New York City, in particular, struggled to stop soaring infection rates and, by July, the death toll in the Big Apple was twice that of entire nations such as China and France.
“I think COVID has been largely associated with urban centers due to issues of population density and crowding,” says Ross Boyce, an infectious disease researcher at UNC. “But I think some of those same risk factors are also at play in rural communities — and that shouldn’t be ignored.”
Nearly 40 percent of North Carolina’s population resides in rural communities, according to the 2010 U.S. Census. Rural communities often have fewer clinics and hospitals, which means less access to testing and treatment, and host major agricultural production facilities with many workers designated “essential.”
Boyce is currently leading a longitudinal study in Chatham County to understand how and why SARS-CoV-2 is spreading through this population — data that are direly needed since most of the current data rely on “imperfect disease markers,” or information about the disease that’s easier to access but may not tell the whole story.
“We can look at how many people have been admitted to the hospital or how many people have tested positive, but that doesn’t really tell you about the whole community,” Boyce says. “If 80 percent of people don’t have symptoms or only mild symptoms that don’t prompt a hospital visit, then we really don’t know how many people out there have been infected.”
Boyce and his team are randomly selecting households to participate in this study. At their first clinic visit, volunteers give blood and undergo a nasal swab. For the next four weeks, they record symptoms and then go back to the clinic for the same procedures. They will repeat this each month for one year.
“I’ll admit, it’s a bit of an intense ask,” Boyce shares. “But it’s something we really need people to do.”
[row]
[column lg=”6″ md=”12″ sm=”12″ xs=”12″ ]

Juliana Cortez explains a nasal swab to Doug Brugler while gathering samples for Boyce’s longitudinal study on the transmission of SARS-CoV-2 in Chatham County. (photo by Megan May)
[/column]
[column lg=”6″ md=”12″ sm=”12″ xs=”12″ ]
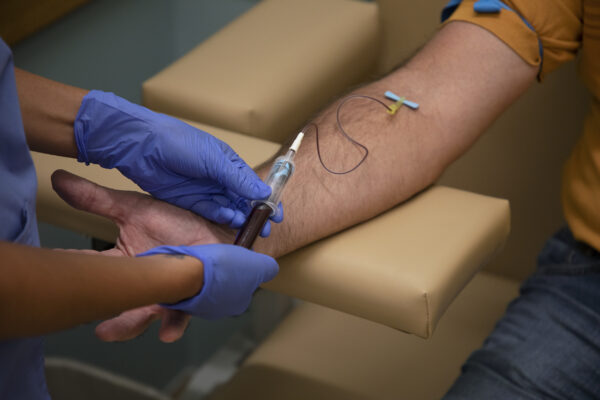
Cortez conducts a blood draw on Brugler for the study, which requires participants to come back to the clinic once a month for one year to give blood and a nasal sample. (photo by Megan May)
[/column]
[/row]
Keeping track of these populations and how the virus affects them, in general, is a hard task. But UNC researchers strive to understand the problems they face and develop solutions to tackle them. While Boyce remains focused on rural populations, others are engaged in projects addressing the needs of additionally vulnerable groups including older adults in assisted living facilities and nursing homes, Latino and African American populations, and people who homeless or at risk of losing their homes.
Nursing homes and assisted living facilities
When the pandemic began spreading across the United States earlier this year, people age 65 and older almost immediately became a target. Assisted living communities and nursing homes were especially at risk, not only because they are filled with people in that demographic, but because such environments rely on caregiving staff who come in from the outside.
“It’s really what’s being brought into these settings. The older adults are helpless victims of this pandemic because they aren’t the ones leaving their home and getting exposed,” says UNC age researcher Sheryl Zimmerman.
Plus, people who live in these places are already vulnerable, points out Anna Beeber, a professor in the UNC School of Nursing. They may have preexisting health conditions or cognitive impairments that create safety issues. Oftentimes, these folks need assistance with daily care like bathing, meals, and reminders to take medication.
Today, 41 percent of all COVID-19 deaths have occurred in long-term care settings among residents and workers. Across the country, more than 216,000 residents have contracted the virus, 25 percent of whom have died, according to the Centers for Disease Control.
Zimmerman has spent nearly three decades studying this population and, for more than 20 years, has co-directed the Program on Aging, Disability, and Long-Term Care at the UNC Sheps Center for Health Services Research. In that time, she’s studied the changing dynamics of long-term care. Zimmerman is especially interested in how assisted living communities have fared during the pandemic. Nursing homes offer medical care to residents, while assisted living communities provide supportive care — and the question of whether the latter needs more access to medical services arises often.
“There’s been discussion that assisted living communities have become places where we need more medical care — and COVID-19 has, perhaps, pushed the envelope,” Zimmerman says.
She and colleagues are collecting information from 250 communities across seven states to answer questions like, did those with some access to medical services experience less outbreaks? How much access did they have to PPE? The pandemic can, hopefully, uncover some of the gaps.
Beeber, on the other hand, is focused on the social aspect of these environments and the importance of visitors for the people who live within these communities. Not only are family members more likely to see subtle changes in the individual resident that could indicate something is wrong, but their presence can also boost the resident’s mood.
“They’re using a lot of creativity to try to keep that engagement,” she says. One community organized hallway bingo and had residents sit in their doorway as a staff member called out numbers in the hall. Others have hosted drive-by parades, where residents sit outside as their friends and family members pull up in their cars for short visits.
Since many long-term care facilities have shut their doors to visitors, this puts the people within these communities at risk for severe social isolation, which can increase depression and anxiety and also impact blood pressure, heart disease, and diabetes.
“We rarely hear about the positive things,” Beeber stresses. “Because the positives are that a community hasn’t had infections or that a staff member tested positive and it didn’t spread to others thanks to good protocols. But we’re not going to hear about that. We’re only going to hear about the nursing homes where multiple residents get infected or have a certain number of deaths. And that is wearing on people who are working so hard to keep these vulnerable older adults safe.”
Staff are also at risk of burnout, Beeber says, as they work day and night to maintain sanitation and safety practices and address the increased needs of residents during this time. Many nursing assistants, in particular, are minorities who are even more vulnerable to contracting the virus. Nationwide, nursing homes employ more than 600,000 nursing assistants, 200,000 of whom identify as Black or African American and about 120,000 were born outside of the United States.
Through 200 interviews with residents, caregivers, and staff members, Beeber hopes to identify how assisted living communities are dealing with social isolation, engagement, and communication during the pandemic.
Black communities in the U.S. and Brazil
Reported COVID-19 cases are 2.6 times higher for Blacks or African Americans, according to the CDC. In North Carolina, African Americans make up 22 percent of the population and, as of September 1, account for 31 percent of COVID-19 deaths. In the state’s seven counties where African Americans make up the majority, five have per capita death rates that exceed the statewide average of approximately 11 deaths per 100,000 people.
In an ongoing study of 446 Black fathers, UNC psychologist Shauna Cooper reports that 139 of them have tested positive for the virus. This may be due to increased exposure at their jobs — 31 percent identify as being high-risk for contracting COVID-19 at work. Fathers working in these environments also are more likely to experience greater family stress, poorer quality of sleep, and an increase in depression and anxiety symptoms, according to Cooper.
“We’ve seen these depictions around families and how they navigate COVID-19 life, and really, it’s a depiction of parents who have been able to work from home,” Cooper says. “That’s not the reality for many families, and Black Americans, in general, are more likely to be essential and frontline workers.”
Cooper has spent her research career studying the impacts of discrimination and how Black families can help their children cope and promote positive development. She has, specifically, focused much of her work on fathers and the role they play in family dynamics and child outcomes.
Cooper is also studying how prior experiences with discrimination may affect Black men in the context of COVID-19. Recent news stories have revealed the anxieties Black men face when they were masks in public, particularly concerns about racial profiling and harassment from law enforcement. In fact, before the pandemic, many states had laws in place prohibiting the use of face masks in public.
“This is something we’ve been telling everyone to do for health purposes. But if you’re concerned that you will be harassed or discriminated against by wearing said mask, that can increase stress for many Black men,” Cooper says.
Kia Caldwell, a professor in the Department of African, African American, and Diaspora Studies, has spent more than a decade studying how racial disparities affect Black people. She focuses on Brazil, a country with extreme income inequality and a population where 54 percent — about 113 million people — identify as Afro-Brazilian. That’s more than twice as many Black people than the United States, where about 43.9 million people identify as Black or African American.
One factor makes this kind of research difficult: Many Brazilian health care providers don’t ask patients to identify their race. They often believe it offensive to ask about these identifiers and will sometimes guess race based on the person’s social class or skin color.
“The data is also spotty here in the U.S.,” Caldwell says. “The CDC was, really, forced to start collecting the data and publishing it more broadly, but it’s still not where it needs to be. Although we’ve seen a lot of reports about African Americans being disproportionately affected by COVID-19 or dying in disproportionate numbers, some of the data is still not very good.”
The problems Afro-Brazilians have dealt with during the pandemic parallel those experienced by African Americans, according to Caldwell. Many are essential employees and work in domestic service, meaning they are housekeepers, nannies, or cooks in people’s homes, which places them in close proximity to a lot of people. A large part of this population lives in favelas, neighborhoods that are densely populated and have poor sewage and sanitation systems. People can’t always wash their hands, Caldwell says.
As a health researcher, Caldwell considers the systems both Brazil and the U.S. have in place. While Brazil has universal health care, it has extreme class divides that determine the level of that care. Middle class and wealthy Brazilians, for example, often have private health insurance that allows them access to private health centers and hospitals. In the U.S., the need for Medicaid expansion often prevents minorities from accessing any care, including tests and treatments for COVID-19.
“What we can learn from Brazil, and also the United States, is that public health is affected by politics,” Caldwell says. “Wearing masks, how seriously things are taken, which populations are allowed to die. When democracy is in peril, it places a lot of other things in danger.”
Food workers and Latin Americans
In August, the CDC reported that Latino people are hospitalized for COVID-19 4.6 times the rate of white people. Like African Americans, they are more likely to have preexisting health conditions such as diabetes, but they are often hesitant to engage with doctors. For some, it’s because they are undocumented; about one-quarter of Latino adults in the U.S. are. Others struggle with the language barrier. Plus, many Latino people are self-employed or work low-wage jobs with minimal benefits and safety protocols.
Consider food-processing industries, recently donned the “Typhoid Mary of this pandemic” by Esquire magazine. Many Latino people work within these environments, particularly the U.S. poultry industry, which has historically hired undocumented workers. Every day, poultry workers stand shoulder-to-shoulder along both sides of a conveyer belt to process chicken.
Poultry is North Carolina’s number-one agricultural industry, bringing in more than $37 billion each year for the state and employing over 146,000 people, according to the North Carolina Poultry Federation. The state is also home to an abundance of hog and cattle farms, so meat processing, in general, is a major economic engine for the region. On a global scale, the United States is the largest chicken and beef producer in the world.
In late April, these jobs were declared essential amidst the COVID-19 pandemic. But, as evidenced above, slaughter and processing work environments make social distancing and sanitation required to keep the virus at bay more difficult. In May, just a few weeks after the executive order was made, the N.C. Department of Health & Safety reported upward of 1,300 COVID-19 cases in 23 meat processing plants. As of September, nearly 500 plants across the nation have been affected, approximately 43,000 workers have tested positive, and more than 200 have died.
When SARS-CoV-2 made its way to the U.S. earlier this year, few meat-processing companies took action to protect their employees. Only after people in the plants began dying did employers start implementing precautions. Some installed Plexiglas — or simply shower curtain — barriers, expanded break areas, and took temperatures of employees as they entered the building. But it wasn’t enough.
Everyone here is already sick, one Guatemalan poultry worker texted UNC anthropologist Angela Stuesse. And without paid sick leave, most of [us] are still at work.
“It was just spreading like rapid fire, and it wasn’t long before this man tested positive,” Stuesse says. “He did go home and quarantine when he was recovering, but he pointed out that a lot of his coworkers were working through their illness. They simply couldn’t afford to stay home. How can anybody protect themselves in these circumstances?”
This demographic has been hit particularly hard by the virus. In July, 45 percent of COVID-19 cases in North Carolina were among people in the Latino community — a number that’s since reduced to 35 percent according to the N.C. Department of Health and Human Services. Regardless, data for the meat and poultry industries are severely lacking. Using existing data from the U.S. departments of Labor and Agriculture and the American Community Survey, Stuesse and sociology PhD student Nathan Dollar are trying to pinpoint the demographics of these workers to aid in reporting efforts.
UNC epidemiologist Natalie Bowman, on the other hand, is leading a project to understand COVID-19 transmission within meatpacking plants and other food-processing facilities. She and her team will focus on Chatham and Lee counties, home of Mountaire Farms and Pilgrim’s Pride, two poultry plants where COVID-19 has spread among workers. In April, 74 Mountaire Farms employees tested positive for the virus. While Pilgrim’s Pride hasn’t reported its number of positive cases, the facility made headlines in May upon the death of one of its workers.
Bowman and her team will not only complete nasal swab testing and collect blood samples of employees who volunteer for the study, but also their household members to try to pinpoint whether the infection began in the plants or somewhere else.
Bowman wants to tease out how much transmission is occurring within meatpacking plants and other workplaces. How much of it is broader community transmission? And how much transmission within food processing facilities places household members at risk as well?
“In this particular population, we’ve already seen outbreaks of hundreds of people, and those outbreaks clearly spillover into surrounding communities,” Bowman says. “So learning how to stop the spread in the workplace is critical. It’s critical from the standpoint of just being able to keep the economy and supply chain moving, but more importantly, to try to keep people healthy.”
People without homes or at risk of losing them
Not everyone can hold a job, though — and that’s something else that needs to be considered during the pandemic. What happens to those without jobs? To people without homes to go to each night?
For the past two years, Antoine Bailliard has worked on a community-based mental health project called HomeLink, which assists people who are homeless or at risk of losing their homes — and who also have serious mental illnesses like severe depression and anxiety, schizophrenia, bipolar disorder, and personality disorders.
“Some of these folks with serious mental illness can have some pretty intense cognitive challenges due to medication side effects, a history of oppression, missed opportunities to develop skills, and other factors related to their illness,” Bailliard says. “So the need for support to perform independent living skills necessary to live in the community is pretty substantial.”
This four-person team includes a social worker, housing and employment specialist, peer support specialist, and an occupational therapist. As an occupational therapist, Bailliard supervises this group, which works with these communities to teach them independent living skills like budgeting and spending, cooking and cleaning, and even safe sex practices.
“If it’s a skill for living independently, chances are we’ve addressed it in some form or another,” Bailliard says.
In the time of COVID-19, those skills have morphed into helping people understand how far away six feet is to properly social distance, the correct way to wear a mask, handwashing, and other public health measures. Staying six feet away is a relatively abstract concept, Bailliard says. One way to teach someone to do that is use something familiar, like their couch. Explain that the couch is the right distance and then tell them to keep a couch-length away from a person. That’s tangible and concrete.
“One thing is certain: Just relying on verbal instruction and telling people to do it just doesn’t stick,” Bailliard says. “People don’t remember. They need reminders. They need visual demonstration. They need a structured plan on what to do when they leave the house.”
Since Bailliard and his team usually make these visits in person, they’ve had to reevaluate their entire program. Instead of meeting inside they meet the client outdoors or in their car and have a conversation through the window. As part of a larger project hosted at the UNC Center for Excellence in Community Mental Health, they are providing smartphones to some of their patients so they can engage in telehealth.
“It’s rough living,” Bailliard says. “And then COVID happens. It exacerbates isolation, boredom, and loneliness — which contribute to instability, symptoms, and hospitalization. It’s the perfect storm for this population.”
A virus that affects us all
While many of these disparities existed before SARS-CoV-2, they have been made more prominent since its spread. But why did it take a global pandemic to bring them into the spotlight?
“A lot of inequities become even more salient in these moments,” says Cooper. “These are not new issues, but the people experiencing them are feeling them differently. We are seeing things unfold in ways that are both similar and distinct.”
Caldwell agrees, adding that these health disparities are now in the spotlight because the high level of illness and death caused by COVID-19 has not been seen in this country in 100 years. So far, the United States alone has more than 6.4 million active cases and 192,000 deaths.
“This makes it harder to deny what is happening or sweep it under the rug,” Caldwell says. “Coupled with this is the fact that COVID-19 is on almost everyone’s mind in the United States, so we are all paying close attention to it.”