Robots that mimic human skin. A wearable patch for wireless drug delivery. A device that can communicate with 3D cell structures called organoids.
These sound like something from a science-fiction novel, but they are the real projects of Wubin Bai. As a professor of applied physical sciences at UNC-Chapel Hill, Bai works with soft and nanomaterials to create next-generation medical devices.
Soft materials are “anything we can deform with our hands,” he says. These include foams, gels, liquids, plastics, and biological materials like organs and cells. Nanomaterials are teeny-tiny particles less than 100 nanometers in size. Cell components, DNA, and proteins are nanomaterials.
Bai’s lab specializes in combining artificial and biological materials to create new medical devices needed by the health care field. But his background in physics and materials science is just one part of the equation. He often needs the expertise of clinicians, biologists, and other scientists to create these innovations.
“I want to understand the challenges that exist in health care and biology,” he says. “These enormous fields are a goldmine for us to explore.”
Colliding interests
Bai’s background is rooted in high-energy physics. During his undergraduate degree at the University of Science and Technology of China, he worked in a particle accelerator facility that smashed electrons together at incredible speeds and studied the types of materials generated from these collisions.
Then, he spent a year as an exchange student in a lab specializing in condensed matter physics research. Bai would compress soft materials into tiny spheres to understand what happens during earthquakes at the quantum — or smallest — level.
“I grew interested in the mechanics of soft materials and what they could achieve,” he explains. “A simple modification in molecular structures and compositions can make them super stretchable or strong and rigid. That wide range of properties provided a fascinating toolbox for choosing materials and tailoring them to our application.”
Bai went on to pursue a PhD in materials science and engineering from the Massachusetts Institute of Technology and then a postdoctoral research position at Northwestern University. In 2021, he started his faculty position at Carolina.
“It’s quite exciting at UNC, where there’s a strong interest in multidisciplinary collaboration and platforms cultivated by leadership to facilitate these solution-driven collaborations,” he says.
Improving treatment and patient monitoring
Today, Bai is involved in numerous projects at Carolina.
One is a wireless patch that delivers drugs to patients using a smartphone or computer. About the size of a Band-Aid, the patch contains microneedles that deliver medication into the patient on-demand.

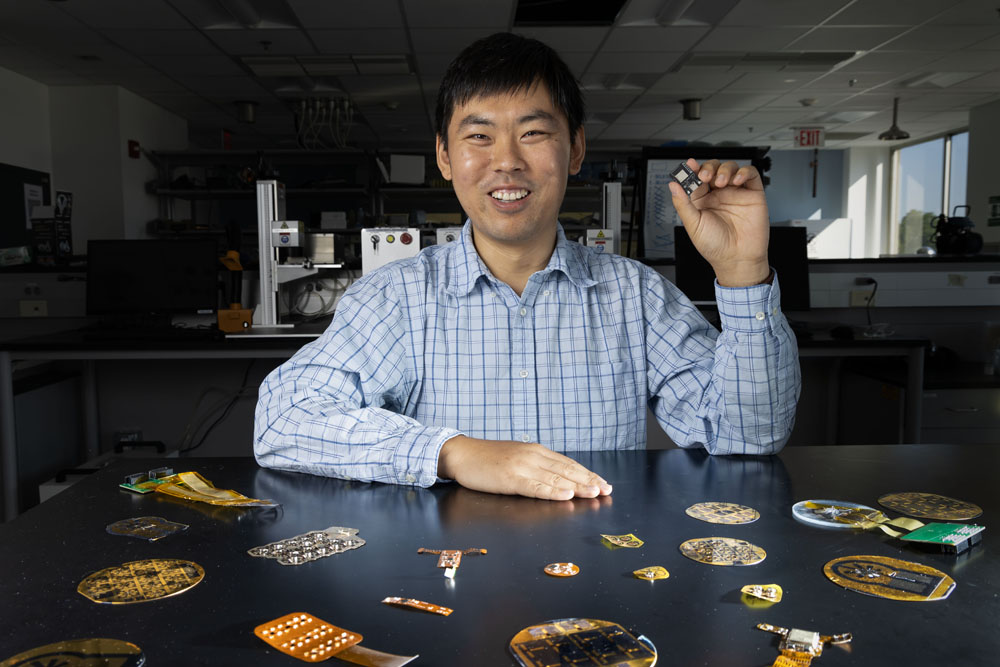
Bai holds a wearable skin patch that can continuously measure blood oxygen levels, heart rate, respiration, and blood pressure. (photo by Alyssa LaFaro)
Bai and his collaborator, pharmacologist Juan Song, believe the patch could administer multiple medications at once, making it useful for diseases like Alzheimer’s and HIV, which require a cocktail of drugs to treat. While it has already received a provisional patent from the U.S. Patent and Trademark Office, Bai admits that they still have challenges to address, like an effective way to refill the drugs within the patch to make it more sustainable for long-term use.
Another is a pulse oximeter that can provide more effective readings for patients of color. Because only a small range of skin tones were considered in the creation of these devices, some readings can be inaccurate.
“So we’re designing a spectrometer that incorporates a broad range of light sources to consider multiple skin tones,” Bai says.
Spectrometers measure the amount of light absorbed by a chemical substance. In oximeters, they measure oxygen levels in the blood. But current technology can only detect two of the seven light wavelengths. The new device will use infrared and other lights to improve the accuracy of readings.
Recently, Bai and his team realized that this technology goes beyond pulse oximeters. Infrared light penetrates deep into the body and gets absorbed mostly by muscles, which means it can be used to track subtle muscle movement — from the heart to the stomach — without invasive probes.
In response, Bai’s lab has created another wireless, wearable patch for deep tissue monitoring that allows doctors to track vitals in real-time and improves comfort in patients. Current deep tissue monitors often require implantation using ultrasound technology.
“We could put it near the neck to monitor coughing and swelling in the throat without any painful intubation measures,” he says. “We can do long-term monitoring, and we’re thinking about how we can extract more conclusive information using machine learning, which looks promising.”
Accessing hard-to-reach places
While most of these devices work outside the body, Bai and his collaborators in biology, biomedical engineering, and chemistry are also developing technology for use inside the body: robots that mimic human skin.
This e-skin uses silver nanowires and conductive polymers to sense its surroundings and adapt as needed. It can mold to the organs it’s treating, administer treatments like electrical signals, and take a variety of measurements such as blood pressure and bladder volume.
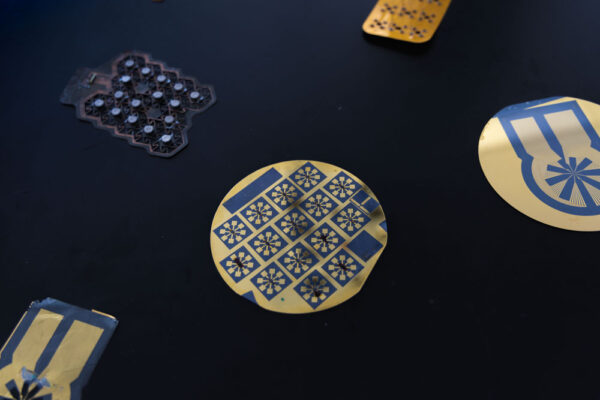
Some of Bai’s tiny devices: a wearable patch to map skin mechanics (upper left), a series of multimodal transistors using 2-dimensional materials (center), and an array of microelectrodes to record activities from brain organoids. (photo by Alyssa LaFaro)
“I think, in the field, medical implants are what patients are most scared of. And I think they generate more headaches for doctors because there’s lots of complications that can occur,” Bai shares.
For example, implants in the brain can be used to stimulate neurons — but they require major surgery and the injection of electrodes into the brain. It can be difficult to find the targets of the electrodes, so surgeons end up extracting and reinjecting them multiple times.
E-skin could be a game-changer for such risky procedures.
That’s why Bai is also collaborating with Carolina geneticist Jason Stein, who creates 3D cell structures in petri dishes — called organoids — that use a patient’s real brain cells to test drugs on to determine best treatments for brain diseases. Bai is helping Stein create a platform to keep these mini-brains alive and monitor their vitals and activities.
Training the next generation
In his three short years at UNC-Chapel Hill, Bai has built a large cohort of young researchers who work in his lab and develop projects based on their own interests. He is currently mentoring more than 30 of them, from high school students to postdoctoral researchers.
“Part of my passion for building a research lab is to offer a platform where young researchers can explore and identify their possible long-term passions,” he shares. “They often bring up ideas and thoughts that are not influenced or molded by previous research in this field. Those refreshing, sometimes out-of-box, thoughts could draw exciting innovations in our research.”
Both Bai and his students are motivated by the pace at which these projects move. Creating powerful medical tools with small, accessible devices drives the production process.
“Our research connects with broad communities and can be translated into the real world,” Bai says. “That motivates us to constantly provide new visions, ideas, and concepts to further revolutionize medical technologies and improve health care.”