Whoosh, whoosh, tick. Whoosh, whoosh, tick.
Soft morning light bathes a man in a white-clad bed. As his chest slowly rises and falls, the rhythmic whirring continues — the sounds of a mechanical ventilator helping him breathe. Eyes open, he looks exhausted but grateful. Hopeful. He survived another night.
Before arriving in this place, he experienced a slow progression of symptoms: a dry cough, chest tightness, shortness of breath, and fever. The last pushed him to visit the hospital, where his symptoms worsened, and his lungs began to fail him. Within hours of arriving, doctors intubated him.
This experience is one many have endured recently. But this is not the present day. This is not COVID-19. It is, though, the start of an epidemic that would change the world forever. The year is 1982. The man suffers from pneumocystis pneumonia (PCP), and doctors have just diagnosed him with a previously unheard of disease that’s slowly infiltrating the population: AIDS.
Like most hospitals, UNC saw its first AIDS cases in the early 1980s. At the time, nearly three-quarters of the people diagnosed with the immunodeficient disease contracted PCP. In 1984, researchers from the Pasteur Institute in Paris discovered HIV as the virus that causes the disease.
One year later, about 15 to 20 percent of all admissions to UNC Hospitals were for AIDS. These patients were placed in a special ward that now serves people with COVID-19. Some of the nurses within the ward are the same ones who helped with the HIV epidemic, says Myron Cohen, director of the UNC Institute for Global Health and Infectious Diseases.
Since HIV became a pandemic, more than 75 million people have been infected with the virus and about 32 million have died from AIDS, according to the World Health Organization. Thirty-eight million people are still infected worldwide.
Epidemic vs. Pandemic
An epidemic, according to the Centers for Disease Control, is an unexpected increase in the number of disease cases within a short period of time. A pandemic is a type of epidemic that covers a larger geographic region and affects a high proportion of the population. HIV and COVID-19 are both pandemics, with people infected all over the world.
Today, HIV researchers have another nasty virus to contend with: SARS-CoV-2. To date, nearly 12 million people have been diagnosed with COVID-19, half a million people have died worldwide, and one-quarter of those deaths have been in the United States.
But there is much hope — in part, thanks to Carolina’s prowess in the field of HIV.
“Virtually every HIV expert on this campus has been assigned or repurposed, in one way or another, to work on COVID-19,” Cohen says, “because they are able to deal with emerging pathogens after dealing with HIV for 30 to 40 years.”
Of the top 10 universities conducting the most HIV research in the world, UNC places at number three, a designation the university has achieved thanks to years of hard work across all aspects of the field, from prevention to vaccine development and, ultimately, a cure.
Changing behaviors
In 1981, while conducting medical evaluations as part of UNC Hospitals’ consultation service, Cohen walked into an exam room to find a young, feverish man with hemophilia — a blood disorder that prevents clotting — whose lymph nodes were about the size of a small fist. Doctors tested him for cancer, but the results came back negative. The patient’s health continued to deteriorate at a rapid pace.
This must be AIDS, Cohen thought.
After assessing the severity of the man’s symptoms, hematologist Gil White requested permission to send one of the man’s lymph nodes to a biomedical researcher at the National Cancer Institute (NCI). Cohen’s guess was soon confirmed.
The man soon passed away and, within months, UNC Hospitals’ 30-bed AIDS ward filled to capacity. Between 1981 and 1984, more than 50 percent of the nation’s hemophilia population who received treatments through blood transfusion became infected with HIV.
The beginnings of the HIV epidemic created fear across America. Where did it come from? How does it spread? Who is most susceptible? In response, the federal government placed an AIDS brochure in every mailbox in the nation in 1988.
Other early-stage efforts to tackle HIV encouraged changes in sexual behavior like condom use and the closure of “hotspots” like bathhouses. While these endeavors marked the start of slowing the spread of HIV, it would take much more to halt it altogether. But first, researchers needed to learn more about how the virus works.
Parallel Lines: Shifting to COVID-19
Like the AIDS brochure, the government took a similar approach with COVID-19 and mailed an informational postcard in mid-March 2020. To prevent the spread of the virus through behavioral changes, many states issued stay-at-home orders, and public health officials reiterated the need for consistent handwashing and the wearing of masks, plus social distancing, in public spaces.For more than 20 years, UNC epidemiologist Allison Aiello has studied non-pharmaceutical interventions, such as handwashing, for preventing infectious diseases. Handwashing, she stresses, requires practice and persistence. Currently, Aiello engaged in a COVID-19 study to identify risk factors for infection among health care personnel and their household members.
Evolving with the virus
HIV is a retrovirus, meaning it invades a host’s DNA and replicates within its cells. This makes it incredibly hard to find and fight. Even more complicated is the fact that HIV can evolve to hide within the body and infect different cell types. At first, the virus targets CD4-positive T cells, a type of white blood cell responsible for immune response. But when that cell supply gets low, the virus searches for a new home to live in.
That evolution is what Ronald Swanstrom studies. For a long time, Swanstrom worked on protease inhibitor resistance. Protease is an enzyme involved in the maturation of the virus during assembly, allowing it to become infectious and spread. If you can inhibit protease activity, you can prevent the replicating virus from infecting other cells. While there are more than five protease inhibitors on the market, they must be taken in combination with other antiviral drugs to halt HIV infection.
“Otherwise, the virus begins to mutate and figures out how to keep growing in the presence of the inhibitor,” explains Swanstrom, who adds that understanding these basic biological processes helps improve treatments for the disease.
Swanstrom also researches how the virus gets inside of and functions within the brain — a place with minimal CD4-positive T cells, meaning the virus must learn to adapt there by infecting different cell types. The virus travels to the brain within immune cells and is then forced to evolve for survival. While HIV infections in the brain are often only recognized late in the disease, it’s vital look for the virus here, as it can cause a slew of neurocognitive problems and, in extreme cases, dementia. HIV-associated dementia occurs in approximately 25 percent of people with untreated HIV infection.
“HIV launches an ongoing battle between the virus and the body — and the virus has the advantage that it can evolve rapidly,” Swanstrom says. “So the more we understand what those evolutionary signatures are, the more we understand that interaction between the virus and the host.”
Parallel Lines: Shifting to COVID-19
Much like HIV, SARS-CoV-2 has the potential to evolve, but as it infects a person for only one to two months, little evolution occurs. While the lungs and throat are the coronavirus’ main targets, it can attack human blood cells throughout the body and cause blood clots and stroke. It is not a retrovirus, but it does use RNA to replicate. Ronald Swanstrom and his lab are using their expertise to test potential therapeutics for treating COVID-19.
Searching for a treatment
From 1981 to 1990, AIDS took the lives of more than 100,000 people in the United States. Overall, the average life expectancy following an AIDS diagnosis was one year.
In 1987, a drug called azidothymidine (AZT) gained approval from the U.S. Food and Drug Administration for treating AIDS. First developed in 1964 as a potential cancer therapy, AZT was shelved until the 1980s, when researchers began experimenting with it.
The drug was tested locally by a company called Burroughs Wellcome, which would eventually form GlaxoSmithKline — a key partner of what’s now the UNC HIV Cure Center. Early lab studies showed that AZT could suppress HIV replication without damaging healthy cells. This is called antiretroviral therapy.
AZT seemed to work well at first and was even called “the light at the end of the tunnel.” But it only partially stopped HIV from replicating and produced awful symptoms like bone marrow depletion and anemia.
“It wasn’t very potent, and the virus became resistant,” says Joseph Eron, chief of the UNC Division of Infectious Diseases. Eron began his study of HIV upon graduating from medical school in the mid-1980s.
After coming to UNC in 1992, Eron began working on clinical studies for the virus. He was part of the team that combined AZT with another drug called lamivudine (3TC) — the first “cocktail” that really staunched the virus replication. But, just as Swanstrom’s work on virus evolution suggested, the virus eventually became resistant to that combination, too.
At this time, according to Eron, AIDS was the leading cause of death for men aged 20 to 50 in Durham County.
In 1996, a team of clinical researchers from four sites across the U.S. and their pharmaceutical partners tested a three-drug combination that stuck: AZT and 3TC, plus a protease inhibitor called indinavir. Eron led the treatment study for this therapy at UNC, which was one of the first sites to test its effectiveness.
“This triple-combination therapy really changed HIV from a story of ‘everybody dies’ to ‘now we have a therapy,’” Eron says.
Eron went on to help make this therapy even more effective, morphing it from a treatment that involved taking about 14 pills three times a day to one pill once a day. The first iteration came out in 2003 and has since become the best solution for people living with HIV.
While the therapies of the 1990s were the first to effectively fight HIV, patients still developed serious complications from immune deficiency, including eye infections that led to blindness or ulcers in the mouth, throat, and esophagus. David Wohl, an infectious disease researcher, joined the university in 1997 to address these problems.
As the medications rapidly progressed, the complications changed, forcing Wohl to roll with the punches. The shift in symptoms included an increase in cardiovascular disease risk and metabolic problems causing abnormal weight gain in the belly and back, as well as thinning of the face and arms.
“These metabolic complications became a real drag on the progress of our therapies because people were reluctant to take them,” he says. “They felt like they were making a compromise – they’d live, but they’d suffer from these other problems.”
Some patients also contracted a serious viral infection that can cause problems with the digestive system, liver, brain, and nervous system. To help patients deal with these outcomes, Wohl began comparing dosing amounts and different combinations of antiretroviral therapies to learn if there was a better treatment that could eradicate HIV and reduce these symptoms.
As researchers developed better therapies, symptoms decreased and the focus shifted. While the once-a-day pill continued to work well, it still wasn’t good enough for infectious disease researchers, who are always pushing for a better solution. They soon discovered that the cocktail, though potent, would never clear the entire infection — people needed to stay on treatment for life. The virus, they learned, had another trick up its sleeve: latency.
Parallel Lines: Shifting to COVID-19
Like with HIV, Joseph Eron believes treatment of COVID-19 will be most effective if applied early on in the disease. He leads the AIDS Clinical Trial Group, which has been tasked by the NIH to expand its focus to include treatment of SARS-CoV-2. His team is working in collaboration with Wohl, coronavirus expert Ralph Baric, and pulmonary medicine specialist Billy Fischer to start an outpatient trial for an antiviral drug called EIDD-2801.
Exposing invisible problems
Unlike most viruses, HIV can lie dormant within a person’s cells for a long time. In the early ’90s, researchers found that it continues to replicate even when a person is asymptomatic. But it wasn’t until the early 2000s that they uncovered the virus’s ability to create a reservoir inside individual T cells, where it stays silent until antiretroviral therapy is interrupted.
During that time, David Margolis submitted his first grant to study HIV latency. But his request for funding was quickly rejected. “The agency told me it was well-known that HIV is an active infection, and that there is no latent state of HIV,” Margolis says with a laugh.
Six or seven applications later, Margolis got his funding.
“One of the things we found led to the idea that you could use a drug to specifically reverse latency, to reverse the molecular mechanism that keeps the virus turned off and turns the virus on,” Margolis explains. “The first drug study to try to reverse latency in people was published the day I arrived at UNC in 2005.”
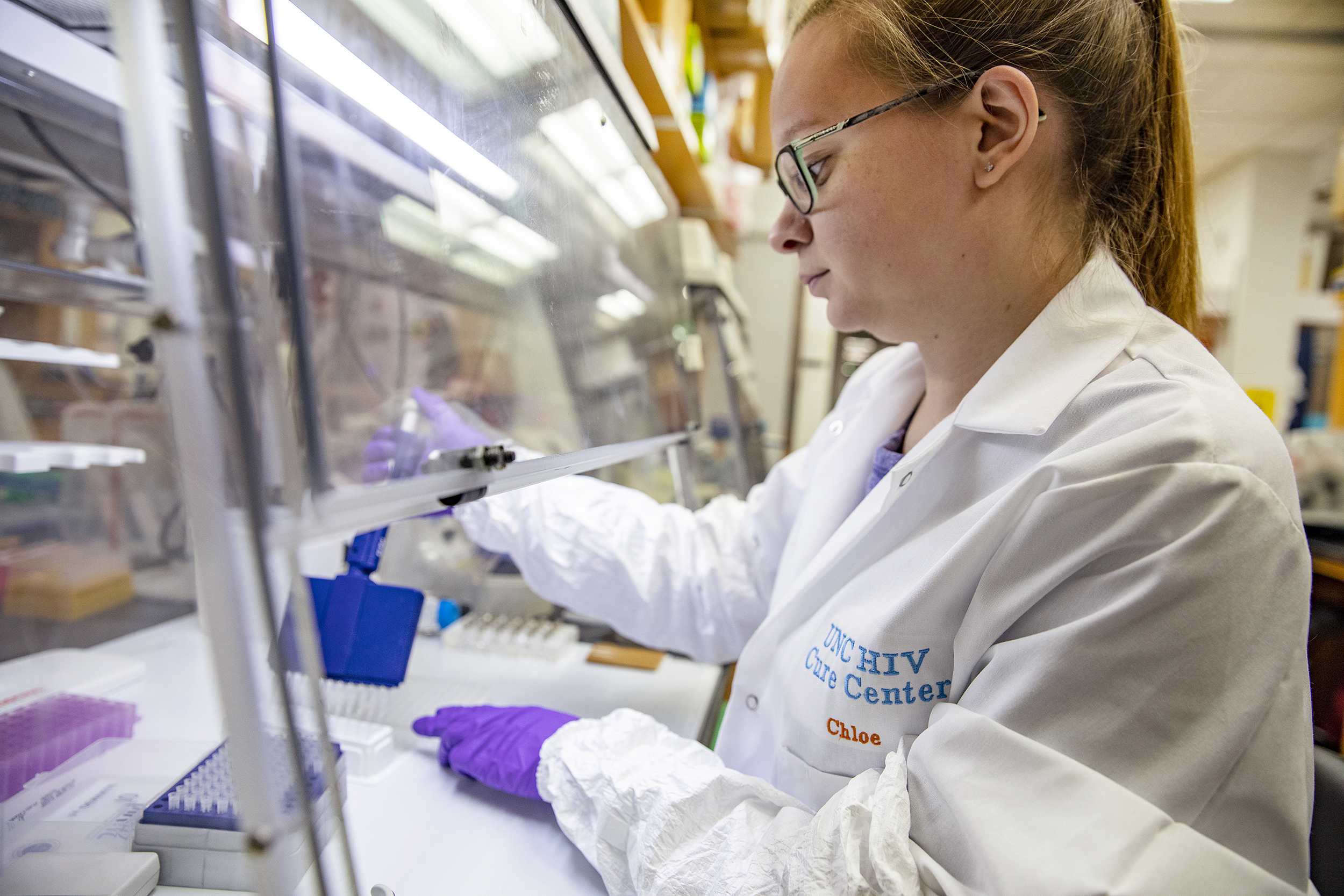
Today, Margolis runs the UNC HIV Cure Center, focused on finding a cure for HIV and AIDS. Understanding and combatting latency is considered a vital step toward developing a cure. Most recently, Margolis, Carolina researcher J. Victor Garcia, and others successfully activated HIV production within latent cells in an animal model. Pushing HIV out of latency means that it’s visible to the immune system and the antiretroviral therapy trying to eradicate it.
The virus also disproportionately affects underrepresented communities. Wohl focused on the prison system and how incarcerated individuals are affected by HIV infection. He and his collaborators discovered that people received more access to treatment while incarcerated and were better equipped to keep the virus at bay. Upon release from prison, that level of care changes as people struggle to find accessible and affordable health care.
HIV infection rates tend to be higher among people living in poverty, people of color, and other vulnerable populations. In fact, HIV affects Black heterosexual women more than women of any other race or ethnicity, and more than 40 percent of new HIV infections occur among African Americans. This is the focus of Ada Adimora, an infectious disease doctor who researches HIV prevalence among women and minorities.
Adimora — who came to UNC in 1989 — has, more specifically, researched how poor health care policies fuel HIV disease disparities among African Americans. She believes more blood tests and surveillance, more economic investments, the removal of polices affecting racial inequality and discrimination, and better sex education programs are all essential societal-level changes that could slow the spread of HIV within this population.
Parallel Lines: Shifting to COVID-19
Numerous investigators within the UNC Infectious Diseases Division are using their backgrounds and technical expertise to help accelerate research and testing of COVID-19 samples. David Margolis is involved in clinical trials to treat COVID-19 patients. “This isn’t the first time HIV research has helped tackle other problems,” says Margolis, who adds that HIV aided the development of potent therapies for hepatitis C.Like HIV, COVID-19 is more prevalent among vulnerable populations. African American and Latinx communities, in particular, have been largely affected.
Building a program
In 1990, Cohen took over as chief of the UNC Division of Infectious Diseases. Eron, who became chief of the division in 2019, recalls sitting in a car with Cohen at the airport after completing his interview for a job at UNC. Before that moment, he was set on accepting a job offer at another university.
“He literally stopped the car in the parking lot and wouldn’t let me out,” Eron chuckles. “He just talked to me for 45 minutes about why UNC was the place I should come to. It was persuasive and compelling and clear that he was committed to me and the HIV work that we were going to do.”
Cohen and Eron played a large role in recruiting Angela Kashuba, who joined the Eshelman School of Pharmacy in 1997 to optimize drug therapies for HIV prevention and treatment and evaluate drugs in early- or late-stage clinical trials. Kashuba, now dean of the pharmacy school, has studied how antiretroviral therapy prevents transmission of the virus, the interactions between drugs, how drugs are distributed throughout the body, and how sex and ethnicity influence the way the body processes drugs.
Cohen is the glue, responsible for bringing in nearly every major player in HIV at UNC.
“I give Mike Cohen a lot of credit,” Swanstrom says. “He really has been our leader in infectious disease.”
Parallel Lines: Shifting to COVID-19
Because HIV is an intracellular virus, Angela Kashuba’s lab specializes in measuring how much of a drug makes its way inside HIV-infected cells. She and her team are completing the same procedures for COVID-19, developing assays to measure drugs for the various studies developed at UNC.
Treating to prevent
Cohen believes these collaborations and the breadth of UNC’s HIV research ultimately led to the creation of a large-scale randomized clinical trial called the HIV Prevention Trials Network 052 (HPTN 052). Formed in 2005 and led by Cohen, HPTN 052 demonstrated that treating an HIV-infected person with antiviral drugs makes them less contagious and prevents transmission to sexual partners — which Cohen and his collaborators termed “treatment as prevention.”
Two thousand heterosexual couples, each made up of one HIV-positive partner and one HIV-negative partner, enrolled in the study. The 2016 results reported a 93 percent reduction in HIV transmission when an HIV-infected person began taking antiretroviral therapy when their immune system was relatively healthy.
“Until we have a safe and effective vaccine for HIV, we must continue to find innovative prevention strategies,” Cohen says.
When the final results of HPTN 052 released in 2016, Cohen oversaw the launch of HPTN 083 — a global study focused on preventing HIV in high-risk populations. Starting in 2012, HIV-negative patients have had access to a once-a-day pill, Truvada, to prevent infection. For this new study, Cohen wanted to compare the efficacy of Truvada to an injectable drug called cabotegravir, which only needs to be administered every two months.
Unlike HPTN 052, HPTN 083 specifically enrolled cisgender men and transgender women who have sex with men — people with high risk of HIV infection. While HPTN 052 focused on the suppression of HIV replication in people infected with the virus, HPTN 083 looks at preventing HIV transmission during sexual intercourse. In June 2020, the study was halted because injections of cabotegravir proved even better at stopping the spread of HIV than Truvada. A companion study called HPTN 084 is currently assessing cabotegravir’s effectiveness for preventing infection in HIV-negative women.
UNC is also involved in testing an alternative to Truvada called Descovy, which avoids the potential negative side effects Truvada can cause in the kidneys and bones, and the Antibody Mediated Prevention study — a first-of-its-kind prevention method that uses anti-HIV antibodies to prevent infection.
While a cure isn’t on the horizon, on a good day Margolis says there might be one in the next five to 10 years.
Cohen believes UNC’s prowess in the field has benefits beyond addressing HIV.
“HIV has taught us how to approach problems,” Cohen says. “It took us literally 20 years to understand the rules of transmission and to become good at some of the things we’re trying to do. For COVID-19, it’s taken us 20 weeks to get to at least some of the same points. This isn’t just a story about HIV. It’s a story about people working together successfully.”